Emergency Physicians Can Improve Patient Care While Supporting Antimicrobial Stewardship
Sponsored Content
SAEM provides this sponsored education as a resource for our members, and does not imply endorsement of the products, resources, or information provided. This content has been developed by bioMérieux.
DIAGNOSING MENINGITIS AND ENCEPHALITIS INFECTIONS IN THE ED
Patients with meningitis or encephalitis have a broad differential diagnosis for the specific underlying causes of the inflammatory responses within the central nervous system (CNS). Properly diagnosing patients who arrive at the emergency room with bacterial
meningitis and viral encephalitis presents a challenge due to how general symptoms may present themselves in early stages.
Because bacterial meningitis can be fatal in healthy people in 24 to 48 hours (Ref.1), time to diagnosis is critical. The right treatment depends on quick identification of the pathogen as bacterial, viral or yeast.
Patients with suspected meningitis are often treated empirically pending diagnostic results (Ref.2 & 3). This can mean lengthy hospitalizations and unnecessary antimicrobial use, all of which add to the overall cost of care while accelerating the spread of antimicrobial resistance.
Potential Barriers to Diagnosing Meningitis and Encephalitis
- Distinguishing viral from bacterial meningitis based on clinical presentation is challenging as patients often present with similar, flu-like symptoms (Ref. 1)
- Although cerebrospinal fluid (CSF) culture is the standard method to test for bacterial meningitis, this method is:
- Time-consuming, taking 24 to 72 hours (Ref.4)
- Technically complex, requiring specific expertise
- Lacking in sensitivity, especially when specimen collection occurs after initiation of antimicrobial treatment (Ref. 2 & 3)
- Unable to detect non-bacterial pathogens, including the most common viral pathogens
- Time-consuming, taking 24 to 72 hours (Ref.4)
- Viral testing may require a molecular amplification method that is time-consuming, often requiring several days for a definitive answer
- Often an expensive send-out test
Rapid Diagnostic Solutions Reduce Time to Diagnosis and Improve Patient Care
Distinguishing bacterial from viral meningitis based on clinical presentation alone is challenging. Obtaining fast, pathogen-specific answers can help save lives and guide appropriate therapy.
Rapid diagnostics help:
- Reduce duration of acyclovir (Ref.4)
- Modify empirical therapies sooner in favor of more specific treatments (Ref.5)
- Reduce length of hospital stay by quickly identifying enteroviral meningitis (Ref.5)
- Reduce patient and treatment costs (Ref.5)
- Enact timely infection control measures (Ref.5)
DIAGNOSTIC SOLUTIONS FOR MENINGITIS AND ENCEPHALITIS INFECTIONS IN THE ED
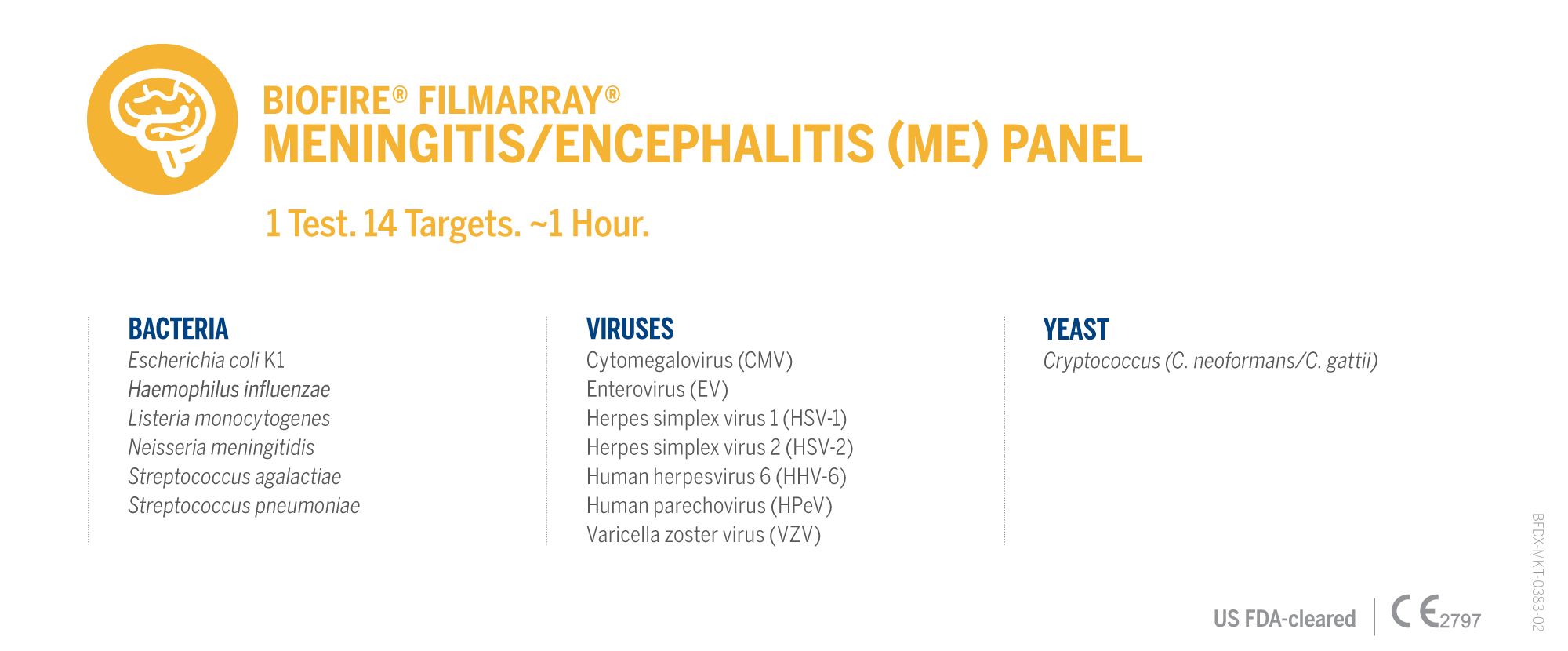
BIOFIRE® FILMARRAY® Meningitis/Encephalitis (ME) Panel enables clinicians to optimize patient treatment for meningitis and encephalitis and select the most appropriate antimicrobial therapy in accordance with antimicrobial stewardship principles.
The BIOFIRE ME Panel is a syndromic multiplex PCR test targeting a comprehensive grouping of pathogens that could be causing a specific syndrome. By targeting pathogens and antimicrobial resistance genes at the molecular level, syndromic infectious disease testing is more sensitive than culture methods and more efficient than a serial approach involving individual and send-out tests.
Traditionally, diagnosing a bacterial infection depends on growing the organism in culture, which can be slow and even ineffective. A syndromic PCR test can detect bacteria in a sample within hours instead of days, even if the organism is difficult to grow or nonviable. Determining the cause of a viral infection, even if there is no specific treatment for it, can help healthcare providers avoid unnecessary antibiotics, reduce hospital length-of-stay, and improve patient satisfaction.
The BIOFIRE ME Panel also detects parasites and fungi for relevant syndromes, which helps healthcare providers determine a causative agent sooner to avoid guesswork and downstream testing. Additionally, identifying antimicrobial resistance genes can promote antimicrobial stewardship and facilitate more informed patient management decisions.
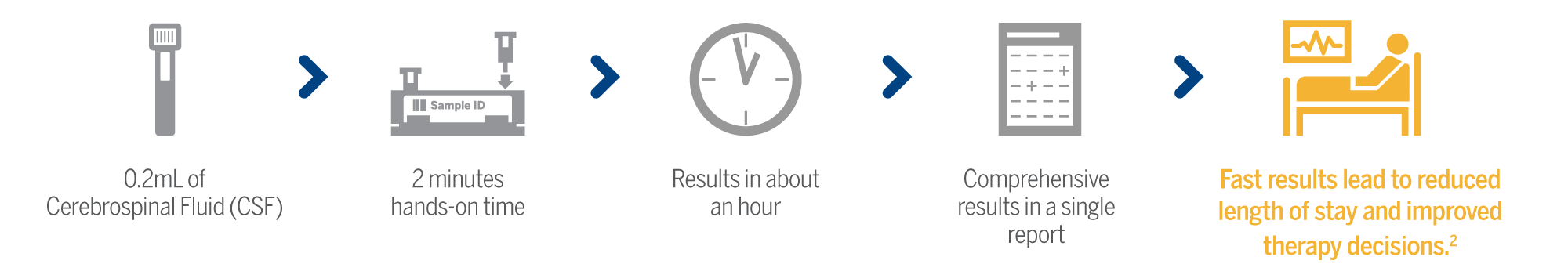
The BIOFIRE ME Panel provides pathogen-specific results in about an hour and can help healthcare providers rapidly distinguish between bacterial and viral meningitis and optimize life-saving therapy.
BIOFIRE FILMARRAY ME PANEL
The BIOFIRE ME Panel tests for a comprehensive set of 14 of the most common bacterial, viral, and fungal pathogens associated with CNS infections in about 1 hour using only 0.2 mL of CSF.
Shorten time to diagnosis*
- 3.3-day reduction for adult patients (Ref.5)
- 4-day reduction for pediatric patients (Ref.2)
*From time of initial presentation to the Emergency Department
Impact antimicrobial therapy
- 2-day reduction in both acyclovir and antibiotic duration for adult patients (Ref.6)
- 2-day reduction in both acyclovir and antibiotic duration for pediatric patients (Ref.7)
Shorten hospital stays
- 2.2-day reduction in length of stay for adult patients (Ref.6)
- 2-day reduction in length of stay for pediatric patients (Ref.2)
Learn more about the BIOFIRE ME Panel at the BIOFIRE website.
ANTIMICROBIAL STEWARDSHIP IN THE EMERGENCY DEPARTMENT
The emergency department (ED) is a critical setting for antimicrobial stewardship efforts, given the frequency of infectious disease encounters and its major role in hospital admissions and acute care outpatient encounters (8). EDs are often the first place where patients with infectious diseases come into contact with the hospital. In this setting, antimicrobial treatment is typically delivered empirically, generally in the absence of microbiological results or feedback regarding patient course and outcomes (9).
YOUR ROLE in Antimicrobial Stewardship
While everyone has a role to play in antimicrobial stewardship, healthcare professionals and clinicians are at the forefront of the fight against antimicrobial resistance. Biomarkers offer clinicians objective information that, along with clinical assessment, help them decide if and when they can safely stop antibiotic treatment. Rapid diagnostic tools support evidenced-based decision making and reduce time to appropriate treatment.
Learn how diagnostic solutions support Antimicrobial Stewardship Programs.
References
- Confederation of Meningitis Organizations Fact Sheet. comomeningitis.org/facts. 2020.
- O’Brien M, et al. Impact of cerebrospinal fluid multiplex assay on diagnosis and outcomes of central nervous system infections in children: a before and after cohort study. The Pediatric Infectious Disease Journal 2018;37:868-71 .
- Bamberger D. Diagnosis, Initial Management, and Prevention of Meningitis. American Family Physician 2010 Dec 15;82:1491-1498.
- Evans M, et al. Impact of the implementation of a rapid meningitis/encephalitis multiplex polymerase chain reaction panel on IV acyclovir duration: multicenter, retrospective cohort of adult and pediatric patients. Diagnostic Microbiology and Infectious Disease 2020;96(2):114935.
- Cailleaux M, et al. Impact of a multiplex PCR assay (FilmArray®) on the management of patients with suspected central nervous system infections. European Journal of Clinical Microbiology & Infectious Diseases 2019;39(2):293-297.
- Moffa M, et al. Impact of a Multiplex Polymerase Chain Reaction Assay on the Clinical Management of Adults Undergoing a Lumbar Puncture for Suspected Community-Onset Central Nervous System Infections. Antibiotics (Basel) 2020;9(6):282.
- Hagen, A., Eichinger, A., Meryer-Buehn, M., Schober, T., & Huebner, J. (2020). Comparison of antibiotic and acyclovir usage before and after the implementation of an on-site FilmArray meningitis/encephalitis panel in an academic tertiary pediatric hospital: a retrospective observational study. BMC Pediatrics, 20(56). https://doi.org/10.1186/s12887-020-1944-2
- Antimicrobial Stewardship in the Emergency Department, Pulia; 2018 Sep 6. doi: 10.1016/j.emc.2018.06.012: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7094813/)
- (Antimicrobial stewardship in the emergency department: characteristics and evidence for effectiveness of interventions, Clinical Microbiology and Infection Volume 27, Issue 2, February 2021, Pages 204-209, https://doi.org/10.1016/j.cmi.2020.10.028)


