Management of the Geriatric Trauma Patient
Authors: Jonathan Henricks, MD, Hussam Salhi, MD PhD, and Lauren T. Southerland, MD
Edited By: Angel Li MD; Shan Liu, SD
Updated: 9/24/2021
Abbreviations Table:
TLS: Advanced Trauma Life Support
GCS: Glasgow Coma Score
MVC: Motor vehicle collision
EMS: Emergency medical services
HR: Heart Rate
CAD: Coronary artery disease
COPD: Chronic obstructive pulmonary disease
IVC: Inferior
Vena Cava
FAST: Focused Assessment of Sonography in Trauma
Case Study
Case Study: A 77 year-old female is brought to the emergency department by EMS for evaluation after a single-car MVC which occurred just prior to arrival. The patient was driving down a back road when she “couldn’t lift the foot off of the gas” and accelerated into a tree with airbag deployment. She is alert and talking to you, currently reporting a headache, neck pain, and left hip pain. Per EMS, vitals are notable for an irregularly irregular heart rate but otherwise “within normal limits.” Per EMS, the patient stated that she takes Coumadin, Metoprolol, Lisinopril, and Hydrochlorothiazide. She is unsure of the year or her current location. The patient’s daughter is en-route to the ED at this time.
Objectives
By the end of this module, the student will be able to:
- Describe a focused rapid assessment of the geriatric trauma patient using an organized primary and secondary survey.
- Discuss the criteria for trauma activation.
- Discuss concerns for geriatric pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures.
- Describe geriatric considerations for the secondary survey.
- Describe how to stabilize a trauma patient and prioritize resuscitative measures.
Introduction
Trauma in the older patient, otherwise known as geriatric trauma, is important to delineate because despite a lower rate of unintentional injuries, these patients have significantly higher mortality and poorer functional outcomes when compared with their younger counterparts (2). Like all trauma patients, the basic ATLS (Advanced Trauma Life Support) algorithm serves as the framework patient evaluation, treatment, and disposition, however geriatric patients are often more complicated than younger adults, presenting a unique set of challenges to the emergency physician.
Currently, there is no standard definition of the term “geriatric trauma,” however in this discussion, we are referring to patients ages 65 and older.
The US Census Bureau projects that the population of Americans greater than or equal to 65 years old will increase from 15% in 2016 to 21% in 2030, due to the aging of the “Baby Boomer” generation (1).. Currently, unintentional injury
(trauma) is the seventh leading cause of morbidity and mortality in the geriatric population, and, amongst these, falls are the leading cause (2, 3). Geriatric patients represent roughly 30.75% of all trauma patients in the US (4) and these patients
have worse clinical outcomes when compared with younger patients (5). The case fatality rate of those aged 75 to 84 (6.66%) is roughly double that of younger adults between the ages of 35 and 44, and even in cases where immediate mortality does not occur,
geriatric patients who experience traumatic injuries have increased mortality within the next 12 months (6).
Initial Actions and Primary Survey
Trauma Activation
While in some cases, the decision to “activate a trauma” is relatively straightforward (eg. A multi-vehicle MVC with loss of consciousness, a fall from significant height, and a GSW to the abdomen), trauma in the geriatric patient may not be quite as obvious. As mentioned earlier, falls, even from standing height, are a leading cause of morbidity and mortality in the geriatric population, highlighting the dramatic physical and physiologic differences that a few decades can make to trauma patients. Multiple studies have demonstrated both the tendency to under-triage geriatric trauma patients to facilities with insufficient trauma capabilities, requiring early transfer to better-equipped facilities (7-9) A study of 2009-2014 Medicare claims data found that nearly half of older adults with a final injury severity score of 16 or higher (moderately-to-severely injured patients) were under-triaged to a non-trauma center (10). This delays necessary care and may be unsafe for patients, prompting the state of Ohio to derive a set of geriatric-specific prehospital triage criteria that has increased the sensitivity for severe injury in geriatric patients by 32%. These criteria can be found below. Always ask about your hospital’s trauma triage criteria and whether it includes additional parameters for older adults. (11)
Trauma patient greater than or equal to 70 years of age |
If an injured patient has any of the following, they should be transported to a trauma center:
|
Figure 1: Ohio Trauma Triage Criteria for older adults
Modifications to the Trauma Assessment of Older Adults
In general, older adults in good states of health have sufficient reserves to accomplish normal activities of daily living. When stressed by acute trauma or illness, however, their decreased physiologic reserves can result in a rapid progression of tissue hypoperfusion and organ failure, a common cause of death in older patients. Beware of this combination of decreased physiologic reserve and impaired resistance to stressors, also known as “frailty.” Frailty indices may be more predictive of death from trauma than initial injuries or vital signs in this population (12).
Primary Survey
The initial systemic trauma assessment (ABCDE’s) and secondary surveys should be conducted according to traditional ATLS principles as discussed in Chapter “Approach to Trauma.” However, there are special considerations in the approach in geriatric trauma, owing to changes in physiology with aging as well as increased rates of medical comorbidities and medication interactions. Additionally, while rapid assessment and effective resuscitation is generally the goal in managing the acutely ill, it is important to be aware of your patient’s advanced directives or other care-planning documents, as certain treatments may go against their medical wishes, which should be respected. The following are special considerations in each step of the trauma primary survey.
Airway
Conduct a systemic airway assessment, focusing on the ability to mask-ventilate, intubate via endotracheal tube, and possible surgical airway (cricothyroidotomy). Older patients have a higher rate of edentulousness than younger patients. Bagging them with the dentures in facilitates ventilation but remember to remove all dentures prior to intubation to improve first pass success. Additionally, due to underlying arthritic and degenerative changes, or prior surgical fixation, these patients often have reduced cervical mobility and a stiffer TMJ, complicating airway assessment and laryngoscopy. One should not use excessive force when adjusting the patient’s head, as this may worsen, or cause, cervical spine injury. Cervical kyphosis, preexisting neck malignancies or prior surgeries/radiation may distort the normal cervical anatomy, which may make obtaining a surgical airway more challenging. Lastly, post-intubation hypotension is more likely in older adults. Consider volume resuscitation prior to or concurrent with securing an airway.
Breathing
Older patients have many physiologic changes to their pulmonary system including reduced chest wall compliance (due to degenerative disk disease, intercostal narrowing and kyphosis), weakened diaphragm/accessory muscles, loss of lung elastic recoil with increased residual volume, and decreased cough reflex/mucociliary function. In non-intubated patients, it is important to follow respiratory rate closely, as these patients are more likely to tire and decompensate as a result of pulmonary injury (eg. contusion) or aggressive fluid resuscitation. Just the act of immobilizing an older patient flat on the gurney can impair respiration. Consider ramping or elevating the head of the bed (if safe) to limit dependent atelectasis and maximize available lung tissue. Ask if the patient needs multiple pillows to breath easily at night, because this suggests that leaving them flat on the gurney for an hour could result in significant discomfort and difficulty oxygenating.
If an older adult has difficulty breathing due to injuries, use of non-invasive mechanical ventilation (CPAP/BiPAP, HFNC) may improve respiratory parameters and temporize the patient to enable goals of care discussions with patients/surrogates. A trial of positive airway pressure is recommended by the EAST trauma guidelines for pulmonary contusions or flail chest (13) End-tidal capnography is highly recommended for older adults if there is concern for underlying lung disease (COPD, pulmonary fibrosis, or pulmonary hypertension), thoracic injury (rib fractures or pulmonary contusions), or if analgesia and sedatives are provided.
Circulation
The cardiovascular system is significantly affected by aging. Over time, there are physiologic and pathologic changes to the heart including gradual stiffening of the ventricles with diastolic dysfunction, cardiac damage from coronary artery disease (CAD)/myocardial infarction, cardiomyopathy, heart failure, and valvular disease (14, 15). Decreased cardiac receptor responsiveness to circulating catecholamines limits the augmentation of stroke volume in response to increased demand (15). As a result, increasing heart rate may be a primary mechanism of increasing cardiac output to compensate for blood loss. Unfortunately, this too may be impaired due to existing conduction system abnormalities, loss of pacemaker cells with aging, and commonly used negative chronotropic agents (beta-blockers, calcium channel blockers). Ultimately, these changes culminate with a “pseudo-normal” physical exam and vital signs that do not reliably reflect the severity of systemic illness that face our geriatric trauma patients. Because “normal” vital signs are not definitively reassuring in the geriatric population, adjusted parameters for heart rate and blood pressure (HR >90, SBP <110 mmHg) have been posited to avoid relative hypotension and “occult” hypoperfusion, a finding associated with double the odds of death (16). In addition to trending vital signs and reviewing past medical records for baseline levels, trending lactates to assess adequacy of perfusion and resuscitative efforts can serve as a useful adjunct in the medical management of these patients (17). For a summary of vital sign pearls and pitfalls in the elderly, please see Table 1:
| Vital Sign | Special Considerations | Concerning Values | Traditional Trauma Activation Vitals |
| Blood Pressure | Antihypertensives |
| SBP <90 mmHg |
| Heart Rate |
| HR > 90 BPM | HR >120 BPM |
| Respiratory Rate |
|
| RR <10 or >30 |
| Oxygen Saturation | Underlying lung disease may alter patient’s baseline | Baseline may be 88-92% rather than 100% in patients with COPD | Oxygen saturation <93% |
Adapted from Clare D, Zink, K, Geriatric Trauma. Special considerations impacting vital signs in the elderly trauma patient (18).
Table 1: A summary of vital signs in older adults that are concerning for significant injury in geriatric trauma patients and warrant intervention.
Regarding steps in resuscitation, identify and treat all life-threatening bleeding first, per ATLS guidelines. The FAST ultrasound exam can serve as a valuable adjunct in rapid assessment for shock from blood loss, and the subxiphoid view of the heart can give a quick gross assessment of contractility. Volume resuscitation cannot fully compensate for poor cardiac output, whether from baseline illness or injury, so any older adult trauma patient who is hypotensive should have a quick ultrasound assessment of contractility. Resuscitate with isotonic crystalloid or blood as needed. If no clear source of hemorrhage is identified, fluid resuscitation with 500cc aliquots of warmed isotonic crystalloid is recommended, with frequent reassessment to avoid pulmonary edema and fluid overload (19). Point-of-care ultrasound to assess IVC collapsibility or pulmonary B-lines may be useful in guiding fluid resuscitation and assessing fluid status, in conjunction with other physical exam findings. If significant bleeding, hemodynamic instability, or significant injury (eg. unstable pelvis), transfusion with blood products is indicated.
Finally, the number of older adults who are medicated with warfarin or other oral anticoagulants is increasing (20). These medications increase the likelihood of morbidity and mortality when compared to younger patients with similar initial injury severity scores. Be aware of your institution’s anticoagulation reversal policies. Vitamin K with 3- or 4 Factor Prothrombin Complex Concentrates for Warfarin, Protamine Sulfate for Lovenox, and the novel reversal agents Praxbind and Andaxanet Alfa for Dabigatran and Factor-Xa inhibitors may be life-saving. Fresh Frozen Plasma is an alternative to 3-4 factor PCCs, but requires longer infusion times and significant infusion volumes, which may not be tolerated in older adults with congestive heart failure, renal disease, or liver disease.
Disability
A Glasgow Coma Scale is documented as a part of ATLS protocol. However, GCS is not as good a predictor for severity of injury in older adults as in younger adults, as a good GCS (14-15) does not correlate with severity of injury on CT for older adults (21). In addition, baseline neurological function can be complicated by comorbid conditions such as underlying dementia or acute delirium from the injury. As such, all depressed neurological function, including amnesia to the event or confusion should be evaluated as a potentially traumatic brain injury. After immediate stabilization/evaluation, we recommend a delirium screening tool such as the CAM-ICU to test for altered mentation even in a patient with a GCS of 15.
Exposure
Exposure is a key step in the primary survey to assess for other injuries. Remember to do a full skin exam as bruising and lacerations can be easily missed, as can pressure ulcers from prolonged backboard/Cervical collar use. Also, the skin exam can give insight into the cause of a fall or inform concern about elder abuse/neglect as causes of injury (see Chapter “Elder Abuse”). After exposure exam, keep the patient warm. Many older adults experience an age-related decline in thermoregulatory capacity and muscle mass. Oral and axillary temperatures can be less reliable (artificially low) in older adults, especially if the person is mouth breathing due to altered mental status, pulmonary disease, or acute injury. If you have an older adult who is confused or has a low GCS, check a rectal temperature.
| Airway | Breathing | Circulation | Disability | Exposure |
|
|
|
|
|
Table 2: Summary of key points in the initial trauma assessment for older adults
CASE PART 2: Secondary Survey
On primary survey, the patient’s airway, breathing, and circulation appear intact. She is confused but opens eyes and moves all extremities spontaneously. She has no open wounds but does have a moderate hematoma to her left forehead and some contusions to her left knee. She has no evidence of basilar skull fracture but does have cervical spinal tenderness on evaluation. She has pain with passive range of motion of the left hip. Her right lower extremity is noticeably weak on examination.
Geriatric Considerations in the Secondary Evaluation
The stable geriatric trauma patient requires a thorough secondary assessment for both causes of the injury and concomitant medical conditions that may contribute to their current presentation. A special consideration in the older adult is to corroborate the patient’s baseline functional status and living arrangements which may help in final disposition planning for these patients. It is essential to screen all older trauma patients for substance and elder abuse, which are rare but can’t-miss diagnoses in this population (22).
Suggested labs include complete blood count, comprehensive metabolic panel, coagulation studies, lactic acid, urinalysis, cardiac enzymes, and a serum or urine toxicology screen. Obtain an electrocardiogram and place the patient on cardiac monitoring to evaluate for cardiac causes/complications of trauma. Imaging should include plain radiographs of the chest and pelvis at minimum, with computerized tomography being the imaging modality of choice in the stable geriatric trauma patient. The FAST exam has not been studied extensively in this population, but should be included as part of the initial evaluation and repeated as part of ongoing hemodynamic monitoring.
Presentation, Diagnostics, and Management based on System
Closed Head Injury
Traumatic brain injury in the elderly has significantly more morbidity and mortality than in younger patients. Due to underlying comorbidities and polypharmacy, traumatic events including falls are more likely to occur, and the prevalence of anticoagulant/antiplatelet agent use increase the risk of severe intracerebral hemorrhage. Several anatomic changes in the elderly are responsible for an increased risk of subdural hematoma and intraparenchymal hemorrhage vs younger adults. Increased adherence of the dura to the skull along with cerebral atrophy decreases the tortuosity of bridging veins across the subdural space, increasing the risk of tearing when exposed to shearing forces in trauma. Increased subdural space due to cerebral atrophy leads to delayed onset of symptoms, which may lead to delayed presentations to the emergency department, up to 17-74 days in one case series (23). This delay in presentation contributes to the higher morbidity and mortality in the elderly. For more information about the various presentations and management of closed head injury, please refer to the chapter, “Closed Head Injury.”

Figure 1: 74 year old patient fall from standing without neurological deficits found to have minor subdural hemorrhage on initial evaluation. If not evaluated, geriatric patients are at risk for delayed presentation for chronic subdural hematoma.
The diagnostic approach to the closed head injury in geriatric trauma differs from the average standard. Because clinical variables are not sensitive enough to rule out injury and clinical decision rules (such as Nexus and Canadian Head CT rules) are not validated or applicable in the geriatric population, the threshold for obtaining CT head imaging is much lower regardless of neurological presentation. Any older adult with physical signs of head trauma or altered mentation should receive brain imaging to evaluation for intracranial bleeding. The treatment of traumatic brain injury involves rapid anticoagulation reversal, evaluation for need for surgical decompression, and early neurosurgical consultation. Supportive care with glucose control, avoiding hypoxia with supplemental oxygen, head of bed elevation, and BP monitoring/control are also critical initial actions. Patients with moderate to severe TBI will require ICU level disposition with frequent neuro-checks and neurosurgical consultation. Those with normal mental status, no neuro deficits, and a small bleed may be amenable to observation or short stay units for 12-24 hours of neuro monitoring. It is recommended that any geriatric patient with confusion or neurological deficits at minimum has 24 hours of observation with continued evaluation for concussion or evolving intracranial pathology.
Vertebral/Spinal Cord Injury
Osteopenia and age-related changes to disks and the spinal canal place elderly at greater risk of vertebral fractures and spinal cord injury (SCI). A fourth of geriatric patients have cervical stenosis, and 90% of patients older than 60 years have degenerative changes in the C-spine (19). This increases leverage on the spinal column when force is applied, causing increased fracture risk. Three injuries constitute the majority of spinal injuries in the elderly population: central cord syndrome, cervical distraction injuries, and odontoid injuries.
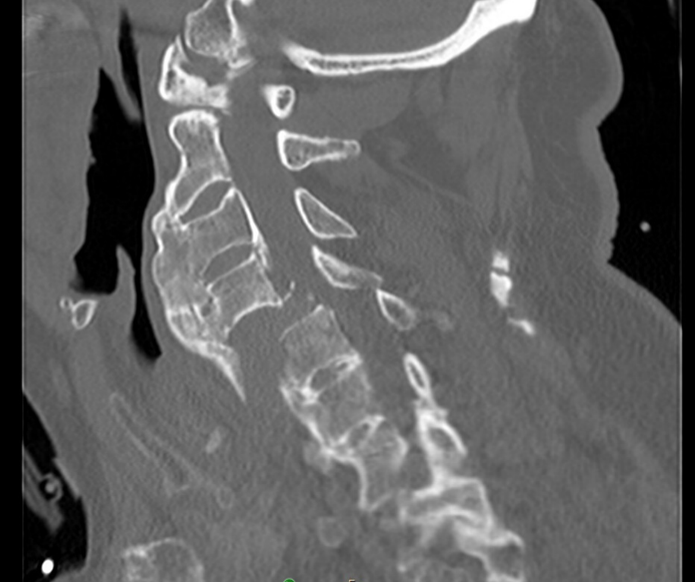
Figure 2: 85 year old male with bilateral jumped facet dislocation, a cervical distraction injury with high morbidity occurred as fall backwards off tipped stool with impact onto neck in flexed position.
As with closed head injury, spinal injuries in geriatric trauma are more difficult rule in or out with physical exam and risk stratification tools (24). Up to 20% of older adults with cervical spine fractures do not report neck pain (25). The location of pain on exam also often does not correlate to the level of injury, and often times a fracture in one section of spine is accompanied by a fracture in another. In fact, up to 26% of geriatric patients with a cervical fracture have been found to have a concomitant thoracolumbar fracture. Therefore, identification of a vertebral fracture in older adults should prompt whole spine imaging. Given the variability in clinical presentation and decreased sensitivity of decision tools for spine imaging in geriatric trauma, liberal CT imaging of the spine is recommended for older adults with spine trauma. In cases of suspected fracture or spinal cord injury, immobilization, spinal surgery consultation, and admission are indicated. Be cautious when empirically placing a cervical collar on an older adult, as they are at higher risk of complications including difficulty breathing, pressure ulcers from poorly fitting collars, and delirium.
Thoracic Trauma
Please refer to Chapter “Chest Trauma” for review of mechanisms of injury, initial management and various presentations of traumatic thoracic injuries. Due to increased rates of osteoporosis and osteopenia, rib and sternal fractures are more common in geriatric patients that suffer chest trauma and can be occult on chest xray. Pulmonary contusions are also very common with minimal trauma, even in the absence of rib fractures. The pain associated with this leads to splinting and atelectasis, which decreases pulmonary clearance and increases the risk of post-traumatic pneumonia, a more common complication in the geriatric population (26).
Chest xray and extended FAST examination, even when combined, have proven inadequate to diagnose thoracic injury in blunt thoracic trauma (27). Thus, CT chest is recommended for all older patients with chest trauma or respiratory complications following a traumatic mechanism. Continuous evaluation and airway monitoring, and early intubation xin anticipation of declining clinical course can be considered. Early pain control with opioid or paravertebral analgesic (rib block) can be instrumental in preventing post-traumatic pneumonia. Chest wall compliance, respiratory muscle atrophy, and capacity for oxygen are decreased with age and cause reductions in VC, FRC, and FEV, limiting the elderly patient’s response to hypoxia and compensation during chest injury. As a result, the threshold for ICU monitoring in elderly patients is lower upon admission with thoracic injuries, especially in the case of multiple rib fractures, pulmonary contusions, and flail chest. In one case series of 401 older adults with rib fractures cared for at University of California-Davis, 63% were admitted to an ICU and a third of those required a critical care intervention or had an adverse event.
Abdominal Trauma
Refer to Chapter “Abdominal Trauma” for review of differential diagnoses, approach, and management of general blunt and penetrating abdominal injuries. Although physical examination helps guide imaging evaluation on secondary survey, the abdominal examination in a significant proportion of geriatric patients can be unreliable. Peritoneal signs may be absent, and reliance on physical examination may lead to missed injuries. There should be a high suspicion for intrabdominal solid organ injury in patients with lower rib fractures or pelvic fractures. As such, CT with contrast is an ideal imaging modality in hemodynamically stable patients to assess the extent of injury. Carefully-selected older adults are candidates for non-operative management (eg. low grade splenic injury) (22). The FAST exam should be part of the initial exam, and can detect large volumes of intraperitoneal fluid and be repeated as a part of hemodynamic monitoring. However, the FAST exam can be “fooled” if the patient has chronic ascites from CHF, liver failure, or ESRD. In these cases, CT with IV contrast can determine if there is active bleeding vs chronic ascites fluid.
Digital rectal exam to assess for intestinal injury, a high-riding prostate (urethral trauma) or spinal cord injury was a part of ATLS secondary exam for many years and is still mentioned in many textbooks. However, this exam has low sensitivity and can also return a false positive in older adults, who have higher likelihood of non traumatic causes of bleeding such as hemorrhoids, diverticulosis, and colonic polyps (28). Rectal tone also is decreased with age and digital rectal exam has a high false negative rate. Unless there is concern for rectal or urethral trauma externally, this exam is unnecessary.
Extremity Injury
Because the geriatric population has a higher rate of decreased bone mineral density and malnutrition with age, they are more prone to extremity injury with lower intensity mechanisms of trauma. The morbidity associated with this can be grave. Isolated traumatic hip fractures in the geriatric population have been found to lead to a 8-30% 1-year mortality (29). Early surgical management of extremity fractures is associated with better outcomes (30). Thus, transfer of hemodynamically stable patients to a center for orthopedic consultation and management is indicated for older patients with traumatic extremity fractures.
Extremity injuries also require different management as compared to younger adults. Older adults may have more difficulties with mobility and activities of daily living if an arm or leg is injured and may require additional support services at home. For example, a younger adult with a distal radius fracture not requiring operative repair can typically be discharged to home safely, but with an older adult you must consider whether the splint will unbalance them, whether they can bathe with only one arm, and whether they use a cane in that hand to walk safely. An older adult with a minor fracture who lives alone can struggle significantly and has a high risk of returning to the ED. In one series, older adults discharged home with isolated forearm fractures had a 10% chance of returning to the ED within 72 hours of discharge (31).
Pharmaceutical Considerations in the Geriatric Trauma Patient
While pharmaceuticals can result in the changes to heart rate and blood pressure, as mentioned above, there are many other classes of medications that may result in impaired primary/secondary evaluations in trauma patients. A list of commonly used agents and their effects on the trauma exam can be seen below:
| Medication Class | Examples | Effects Contributing to Trauma | Effects complicating the trauma exam/care |
| Anticholinergics | Diphenhydramine, Promethazine, Hydroxyzine | Increase risk of falls, confusion, and delirium | Urinary retention, constipation. May cause tachycardia/hypertension |
| Antihypertensives and Diuretics | Metoprolol, Carvedilol, Diltiazem, Amlodipine, Lisinopril, Furosemide | Increased risk of orthostatic hypotension and falls |
|
| Anticoagulants | Warfarin, Aspirin, Clopidogrel, DoACs (Apixaban, Rivaroxaban) | Increased risk of spontaneous bleeding, including intracranial hemorrhage |
|
| Anti-hyperglycemics | Insulins, Sulfonylureas, Meglitinides | Hypoglycemia may precipitate trauma | Trauma patients are often NPO causing iatrogenic hypoglycemia unless dextrose is supplemented |
| Immunosuppressants | Prednisone, chemotherapies, methotrexate | Can contribute to osteoporosis and fragility fractures | Blunts peritoneal irritation, increases risk of wound infection and poor healing. May result in marrow suppression and cytopenias. |
| Opioids | Oxycodone, Hydrocodone, Heroin | Sedative effects may precipitate trauma | Blunted pain response, withdrawal may present with tachycardia. Increased risk of respiratory sedation |
| Sedatives | Benzodiazapines, alcohol, antipsychotic sedatives | Sedative effects may precipitate trauma |
|
Table 3: Summary of medication classes complicating the trauma evaluation and care
Medical Evaluation
Geriatric trauma and falls requiring ED care are sentinel events. While in some cases, these occurrences are truly an accident (eg. Passenger in an MVC or pushed down at a stadium), injuries may be preceded by a medical emergency such as myocardial infarction, stroke, dehydration, pulmonary embolism, sepsis, and intentional- or accidental-pharmacologic overdose. It is important to consider these precipitants when evaluating these trauma patients to appropriately stabilize and treat them in the hospital, as well as in preventing future falls and injuries. Bedside electrocardiogram, cardiac enzymes, urinalysis, and drug screen can be included in the typical trauma workup when deemed necessary to evaluate for these causes. Treatment for these concurrent medical emergencies such as MI and stroke should be made in consultation with appropriate specialists.
Disposition
Once the acute injuries have been identified and treated, a gait assessment and review of fall risk factors should be conducted for all older adult trauma patients whether the mechanism was a fall or not. Combination care provided by trauma and a geriatrics team has been shown to improve care, reduce hospital length of stay, and reduce admission to skilled nursing facilities after a hospital stay for geriatric trauma (32, 33). An observation unit or short stay for physical therapy, geriatrician evaluation, and home safety assessment can also identify and address medical and environmental issues that contributed to their presentation (34, 35). All geriatric trauma patients should be screened for evidence of abuse/neglect, as well as substance use and depression/suicidal ideation as precipitants for their trauma.
| Disposition considerations in geriatric patients |
|
Table 4: Special considerations in the safe discharge of geriatric trauma patients. Adapted from Clare, D, Zink, K. Geriatric Trauma. Emergency Medicine Clinics of North America, 2021-05-01, Volume 39, Issue 2, Pages 257-271, Copyright © 2021 Elsevier Inc
Case Resolution
The patient’s workup is completed. FAST exam negative. CXR negative, and pelvic XR suggests a posteriorly-dislocated left hip with femoral neck fracture. CT head, chest, and abdomen/pelvis are negative for hemorrhage. Spinal imaging suggesting of non-displaced cervical spinous process fracture and concomitant lumbar vertebral compression fracture. A CT Perfusion study was obtained given the patient’s right-sided weakness, showing a left-sided ACA infarct. Labs notable for lactate of 5, hct of 11, and an INR of 2.8. Her anticoagulation was reversed with 4-factor PCC, and she was admitted to the neuro-icu where she received treatment with a mechanical thrombectomy for her stroke, followed by hip reduction and replacement. Due to residual right-sided weakness and new left-sided immobility, she was sent to inpatient rehabilitation for intensive therapy and medical monitoring. She recovered well and was able to return home with support (but no more driving!) 6 weeks later.
References
- Bureau, U.S.C. Projections of the size and composition of the U.S. population: 2014 to 2060 population estimates and projections current population reports. 2017; https://www-census-gov.proxy.lib.ohio-state.edu/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- Trends in causes of death among older persons in the United States, S. National Center for Health, Editor. 2005: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- Stevens, J.A., et al., Self-reported falls and fall-related injuries among persons aged>or=65 years--United States, 2006. J Safety Res, 2008. 39(3): p. 345-9.
- Chang, M.C., National Trauma Data Bank Annual Report. American College of Surgeons, 2016.
- Eagles, D., et al., A systematic review and meta-analysis evaluating geriatric consultation on older trauma patients. J Trauma Acute Care Surg, 2020. 88(3): p. 446-453.
- von Friesendorff, M., et al., Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int, 2016. 27(10): p. 2945-53.
- Garwe, T., et al., Out-of-hospital and Inter-hospital Under-triage to Designated Tertiary Trauma Centers among Injured Older Adults: A 10-year Statewide Geospatial-Adjusted Analysis. Prehosp Emerg Care, 2017. 21(6): p. 734-743.
- Garwe, T., et al., Survival Benefit of Treatment at or Transfer to a Tertiary Trauma Center among Injured Older Adults. Prehosp Emerg Care, 2020. 24(2): p. 245-256.
- Fröhlich, M., et al., Do elderly trauma patients receive the required treatment? Epidemiology and outcome of geriatric trauma patients treated at different levels of trauma care. Eur J Trauma Emerg Surg, 2020. 46(6): p. 1463-1469.
- Uribe-Leitz, T., et al., National Study of Triage and Access to Trauma Centers for Older Adults. Ann Emerg Med, 2020. 75(2): p. 125-135.
- Werman, H.A., et al., Development of statewide geriatric patients trauma triage criteria. Prehosp Disaster Med, 2011. 26(3): p. 170-9.
- Maxwell, C.A., et al., Frailty and Prognostication in Geriatric Surgery and Trauma. Clin Geriatr Med, 2019. 35(1): p. 13-26.
- Simon, B., et al., Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg, 2012. 73(5 Suppl 4): p. S351-61.
- Cheitlin, M.D., Cardiovascular physiology-changes with aging. Am J Geriatr Cardiol, 2003. 12(1): p. 9-13.
- Strait, J.B. and E.G. Lakatta, Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail Clin, 2012. 8(1): p. 143-64.
- Heffernan, D.S., et al., Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma, 2010. 69(4): p. 813-20.
- Salottolo, K.M., et al., A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med, 2013. 21: p. 7.
- Clare, D. and K.L. Zink, Geriatric Trauma. Emerg Med Clin North Am, 2021. 39(2): p. 257-271.
- Walls, R., et al., Rosen's Emergency Medicine: Concepts and Clinical Practice. Ninth ed. 2018.
- Barnes, G.D., et al., National Trends in Ambulatory Oral Anticoagulant Use. Am J Med, 2015. 128(12): p. 1300-5.e2.
- Garza, N., et al., The Increasing Age of TBI Patients at a Single Level 1 Trauma Center and the Discordance Between GCS and CT Rotterdam Scores in the Elderly. Front Neurol, 2020. 11: p. 112.
- Schuur, J.C., Z., Geriatric Trauma, in Rosen's Emergency Medicine: Concepts and Clinical Practice. 2017.
- Chan, D.Y.C., et al., Chronic subdural haematoma during the COVID-19 lockdown period: late presentation with a longer interval from the initial head injury to the final presentation and diagnosis. Chin Neurosurg J, 2021. 7(1): p. 4.
- Goode, T., et al., Evaluation of cervical spine fracture in the elderly: can we trust our physical examination? Am Surg, 2014. 80(2): p. 182-4.
- Healey, C.D., et al., Asymptomatic cervical spine fractures: Current guidelines can fail older patients. J Trauma Acute Care Surg, 2017. 83(1): p. 119-125.
- Battle, C.E., H. Hutchings, and P.A. Evans, Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury, 2012. 43(1): p. 8-17.
- Schellenberg, M., et al., The combined utility of extended focused assessment with sonography for trauma and chest x-ray in blunt thoracic trauma. J Trauma Acute Care Surg, 2018. 85(1): p. 113-117.
- Ahl, R., L. Riddez, and S. Mohseni, Digital rectal examination for initial assessment of the multi-injured patient: Can we depend on it? Ann Med Surg (Lond), 2016. 9: p. 77-81.
- Martinez-Reig, M., L. Ahmad, and G. Duque, The orthogeriatrics model of care: systematic review of predictors of institutionalization and mortality in post-hip fracture patients and evidence for interventions. J Am Med Dir Assoc, 2012. 13(9): p. 770-7.
- Simunovic, N., et al., Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ, 2010. 182(15): p. 1609-16.
- Southerland, L.T., et al., Emergency department recidivism in adults older than 65 years treated for fractures. Am J Emerg Med, 2014. 32(9): p. 1089-92.
- Southerland, L.T., et al., Early geriatric consultation increases adherence to TQIP Geriatric Trauma Management Guidelines. J Surg Res, 2017. 216: p. 56-64.
- Saha, S., et al., Integration of Geriatrician Consultation for Trauma Admissions May Benefit Patient Outcomes. Gerontol Geriatr Med, 2019. 5: p. 2333721419858735.
- Southerland, L.T., et al., An Emergency Department Observation Unit Is a Feasible Setting for Multidisciplinary Geriatric Assessments in Compliance With the Geriatric Emergency Department Guidelines. Acad Emerg Med, 2018. 25(1): p. 76-82.
- Caspers, C.G., Care of Traumatic Conditions in an Observation Unit. Emerg Med Clin North Am, 2017. 35(3): p. 673-683.
