Closed Head Injury
Author: Robert Hsu, MD, Sidney Kimmel Medical College of Thomas Jefferson University
Editor: Roque Ruggero, MD, Texas A&M University College of Medicine, Round Rock campus
Last Updated: November 2019
Case Study
65 year-old female presents after a fall while trying to unload groceries out of her car. She does not recall details of the fall. Her son witnessed the fall and provides his account of the event. She was “just moving a little too fast” while walking up her driveway carrying numerous grocery bags and tripped She fell onto the concrete driveway striking her head and left side of body on the ground. There was no loss of consciousness, but she did seem “dazed” for a few minutes and couldn’t get herself up. She vomited once in the car and a second time on arrival to the emergency department. She has a moderately severe, left-sided throbbing headache. She is experiencing photophobia, lightheadedness, and repeatedly asks her son what happened that brought them to the ED.
On examination, she has a soft tissue contusion to her left parietal scalp without bony deformity. Cranial nerves are intact and she demonstrates no focal neurologic deficit. Her eyes are closed but open to voice. She is conversant but doesn’t know what happened or what day it is. She moves all extremities without complaint. The remainder of her exam is unremarkable.
Objectives
- Calculate a Glasgow Coma Score
- Discuss the various types of head injury
- Decide which patients with head injury require imaging
- Recognize the Cushing reflex and herniation syndromes
- Describe bedside temporizing measures for patients with concern for increased intracranial pressure
Introduction
Head injuries are a common presentation to the Emergency Department. While many are minor requiring no further work up beyond a history and physical, others may be severe and require prompt recognition and treatment to avoid significant morbidity and mortality. The Emergency Physician needs to quickly identify concerning signs and symptoms that require neuroimaging and intervention.
The Glasgow Coma Scale (GCS) is used to define severity of traumatic brain injury (TBI). The score measures the patient’s level of consciousness independent of their specific mechanism of injury. The patient’s best score from each of three categories (Table 1) is added together to determine the final score, which ranges from 3 to 15. Scores of 13-15 are considered mild TBI and are at lower risk for significant morbidity and mortality. Moderate TBI encompasses scores of 9 to 12, with mortality rates of <20% but long-term disability as high as 50%. Scores of 8 and lower define severe TBI with high rates of mortality and long term disability, approaching 40% and 90% respectively. Note that these rates are for isolated head injuries and may differ with concomitant injuries.
Table. 1 Glasgow Coma Scale
Initial Actions and Primary Survey
As with all trauma patients in the emergency department, head injury patients should be evaluated and treated according to the ABCs with a few additional points. Patients with head injury are at risk of concomitant spinal injury. Spinal precautions should be maintained throughout the workup until spinal injury can be excluded, including application of a cervical collar and supine positioning.
The injured brain is extremely susceptible to further injury, and even brief or transient episodes of hypoxia or hypotension may have profound effects on prognosis. A GCS score should be quickly calculated, as all patients with severe TBI (GCS of 8 or lower) require control of their airway and breathing to ensure that hypoxia does not develop as well as to secure the airway to prevent aspiration. Rapid sequence intubation should be performed promptly while maintaining manual in-line cervical spine stabilization. Care should be taken not to hyperventilate the patient, as low PaCO2 levels may cause excess cerebral vasoconstriction and resultant hypoxemia.
Once the airway has been controlled attention should be turned to circulation. Episodes of hypotension result in decreased cerebral perfusion pressure (CPP) which may exacerbate injury. In the equation below, CPP is equal to the Mean Arterial Pressure (MAP) minus Intracraanial Pressure (ICP).
CPP = MAP - ICP
Current guidelines recommend maintenance of a mean arterial pressure 70-80 mm Hg to maintain adequate CPP. This may be accomplished through fluid boluses or vasopressors if necessary. Hypotensive patients should be evaluated for signs of active bleeding, which should be addressed rapidly if identified. If the patient is hypertensive it should prompt assessment for other signs of increased intracranial pressure (ICP) (to be discussed in further detail later in this chapter).
As previously mentioned, a GCS score should be calculated during the primary survey of all head injury patients. Attention should also be paid to the pupillary exam and motor response in all extremities. Abnormalities may be a sign of herniation and require further evaluation (to be discussed in further detail later in this chapter).
Presentation
Once the primary survey is complete and the patient has been stabilized, a full history and physical exam should be performed. The physician should ascertain the mechanism and timing of the injury, any ongoing neurologic symptoms (i.e. alterations of mental status, headache, dizziness, vision or hearing changes, weakness, numbness), or episodes of vomiting. Past medical history and medications should be noted, with particular concern for bleeding disorders or anticoagulants use. Intoxication with alcohol or other substances may complicate the clinical picture. In addition to the GCS and pupil exam performed during the primary survey, physical exam should also include inspection and palpations of any external injuries, looking for step-offs or instability, as well as a full neurologic exam in any cooperative patient.
There are several types of injury that may occur as a result of head trauma:
Epidural Hematoma
An epidural hematoma occurs between the skull and tightly-adherent dura mater. On CT scan this appears as a biconvex (lens-shaped) hyper-dense collection of blood that does not cross suture lines (Image 1). It typically occurs from a blow to the temporal region with disruption of the middle meningeal artery. Because the bleed is arterial it can progress rapidly and requires prompt intervention. The classic presentation consists of a blow to the head with a brief loss of consciousness, followed by a lucid period, then rapid neurologic demise, although this sequence occurs in only a minority of patients.
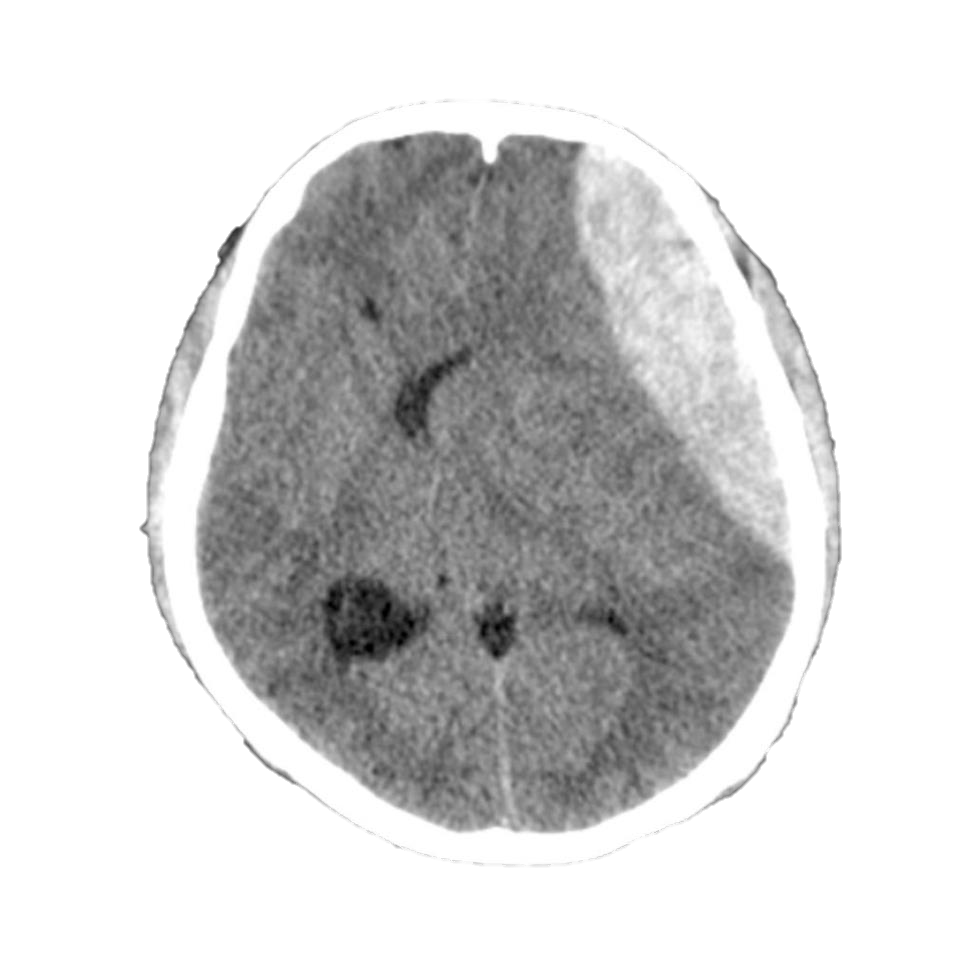
Image 1. Epidural Hematoma. Case courtesy of Dr David Cuete. Used under the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported licence. https://radiopaedia.org/cases/epidural-haematoma-4?lang=us
Subdural Hematoma
A subdural hematoma (SDH) collects between the dura and arachnoid mater, appearing as a crescent shape that may cross suture lines on CT scan (Image 2). Depending on timing, they may appear as hyper-dense (acute, 0-3 days post-injury), isodense (subacute, 3-14 days post-injury), or hypo-dense (chronic, >14 days post-injury). They result from shearing of the bridging veins from a sudden acceleration-deceleration injury. Individuals with high degree of cerebral atrophy, such as the elderly and alcoholics, are at higher risk from this type of injury. As the bleeding is venous, they may progress slowly and not present until days or weeks after the initial injury.
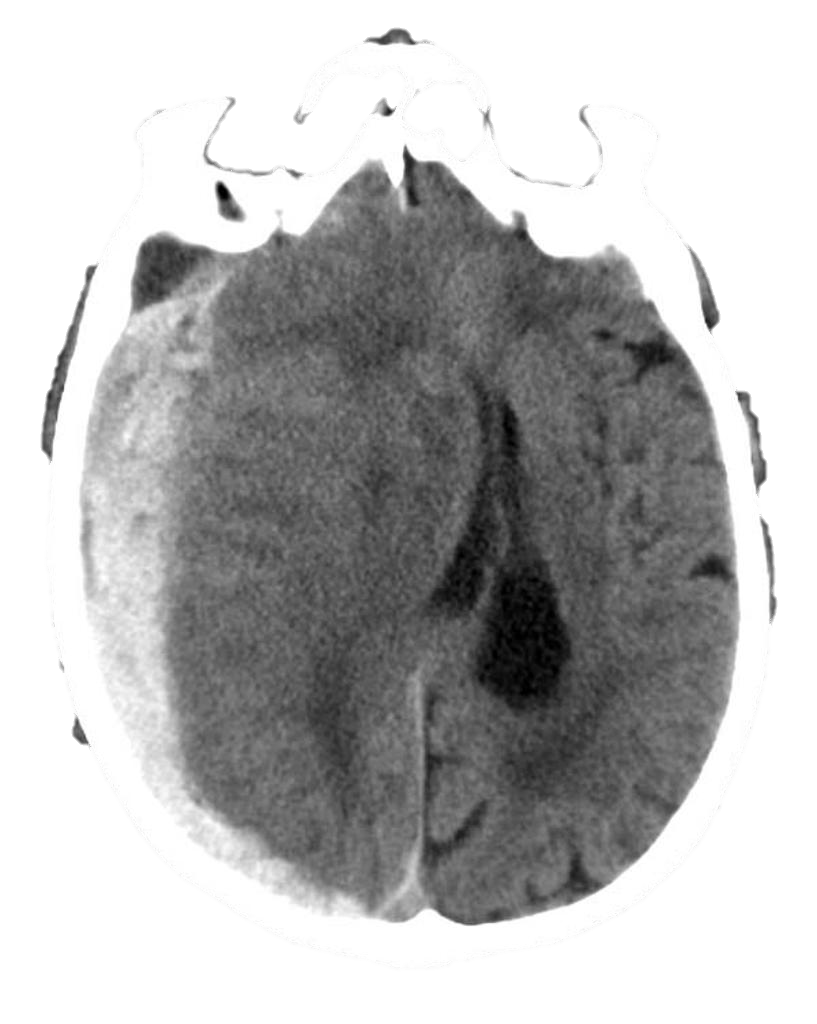
Image 2. Subdural Hematoma. Case courtesy of Frank Gaillard. Used under the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported licence. https://radiopaedia.org/cases/subdural-haemorrhage-acute?lang=us
Acute subdural hematomas typically occur after a significant trauma and may occur in patients of any age. Chronic SDH, on the other hand, occur in those with significant atrophy as a result of minor trauma that the patient may not even recall. Patients will typically present with vague symptoms such as weakness or confusion. A high level of suspicion must be maintained in elderly patients presenting with alterations in mental status or other neurologic complaints.
Traumatic Subarachnoid Hemorrhage
Head injury may also cause bleeding into the subarachnoid space from a disruption of the subarachnoid vessels. This appears as hyper-dense blood within the CSF on CT scan (Image 3). Patients may complain of severe headache, meningeal signs, or photophobia. These injuries may be missed on early CT scans, with improved sensitivity 6-8 hours post-injury.
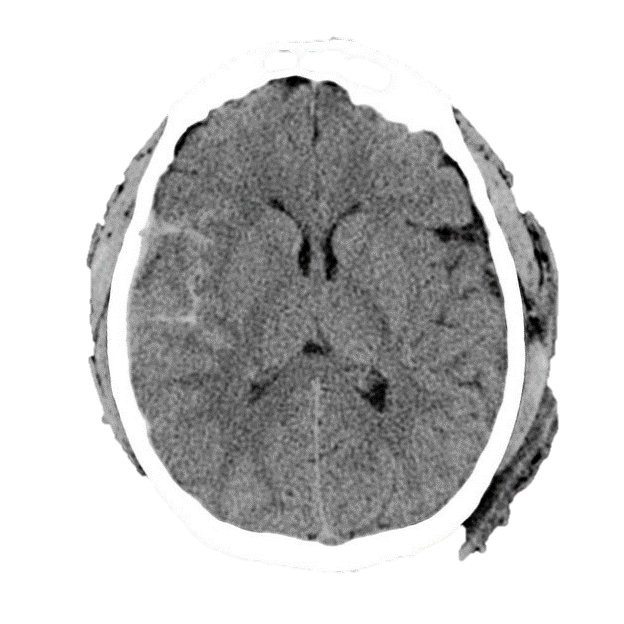
Image 3. Traumatic Subarachnoid Hemorrhage. Case courtesy of Dr Andrew Murphy and Dr. Henry Kipe, et al. Used under the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported licence. https://radiopaedia.org/articles/traumatic-subarachnoid-haemorrhage-1?lang=us
Cerebral Contusion and Intracerebral Hemorrhage
Contusions typically occur in the frontal and temporal lobes or occasionally the occipital lobes. They may occur at the site of trauma or the opposite side of the brain (contracoup injury). Depending on the areas of the brain involved they may present with focal neurologic deficits. Contusions may convert to intracerebral hemorrhage (ICH) several days after the initial injury, so any changes in neurologic status should be investigated by serial CT scans. ICH appears as hyper-dense blood within the brain parenchyma (Image 4).
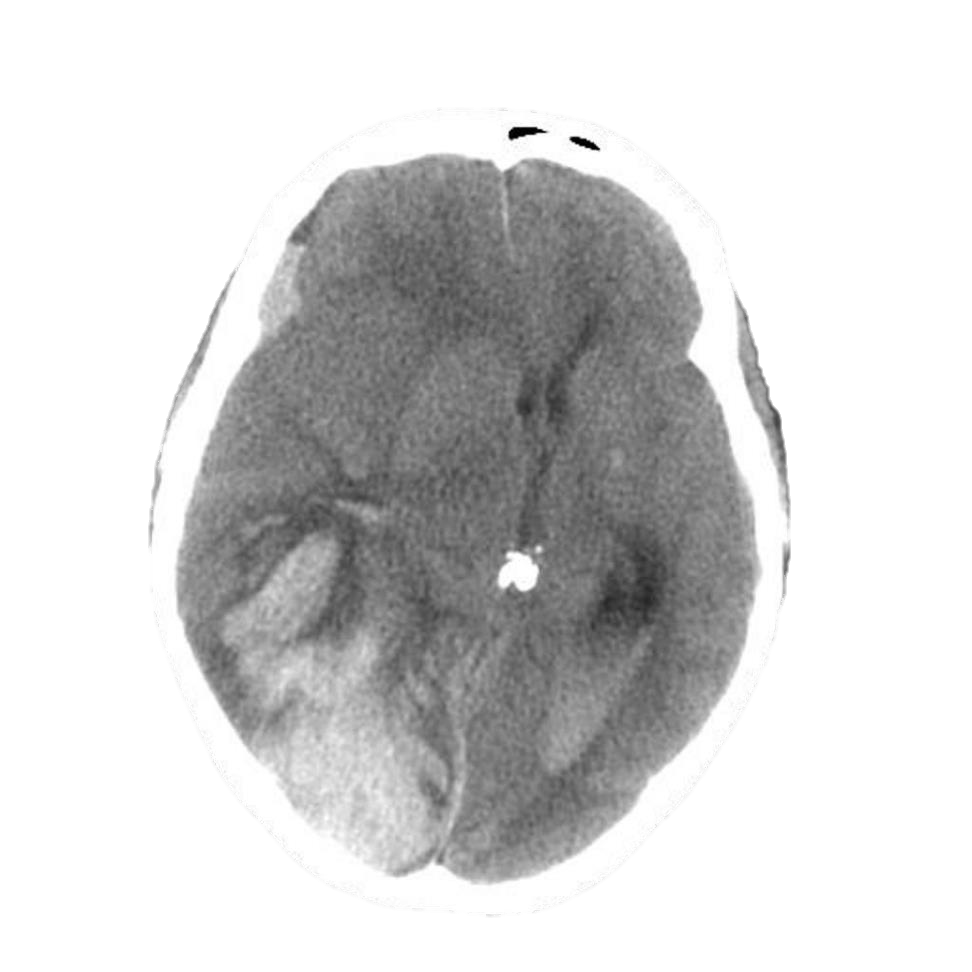
Image 4. Note the large bleed on the patients right (left side of image). Case courtesy of Dr Jeremy Jones. Used under the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported licence. https://radiopaedia.org/cases/intracerebral-haemorrhage-warfarinised?lang=us
Intraventricular Hemorrhage
Intraventricular hemorrhages are rarer in trauma and are associated with worst neurologic outcomes. Primary traumatic intraventricular hemorrhages are more likely associated with coagulopathies and are less common. Secondary intraventricular hemorrhages related to bleeding from intraparenchymal or subarachnoid hemorrhages are more common. These hemorrhages have a worst prognosis due to the forces needed to sustain as well as higher complication rates from increased intracranial pressure.
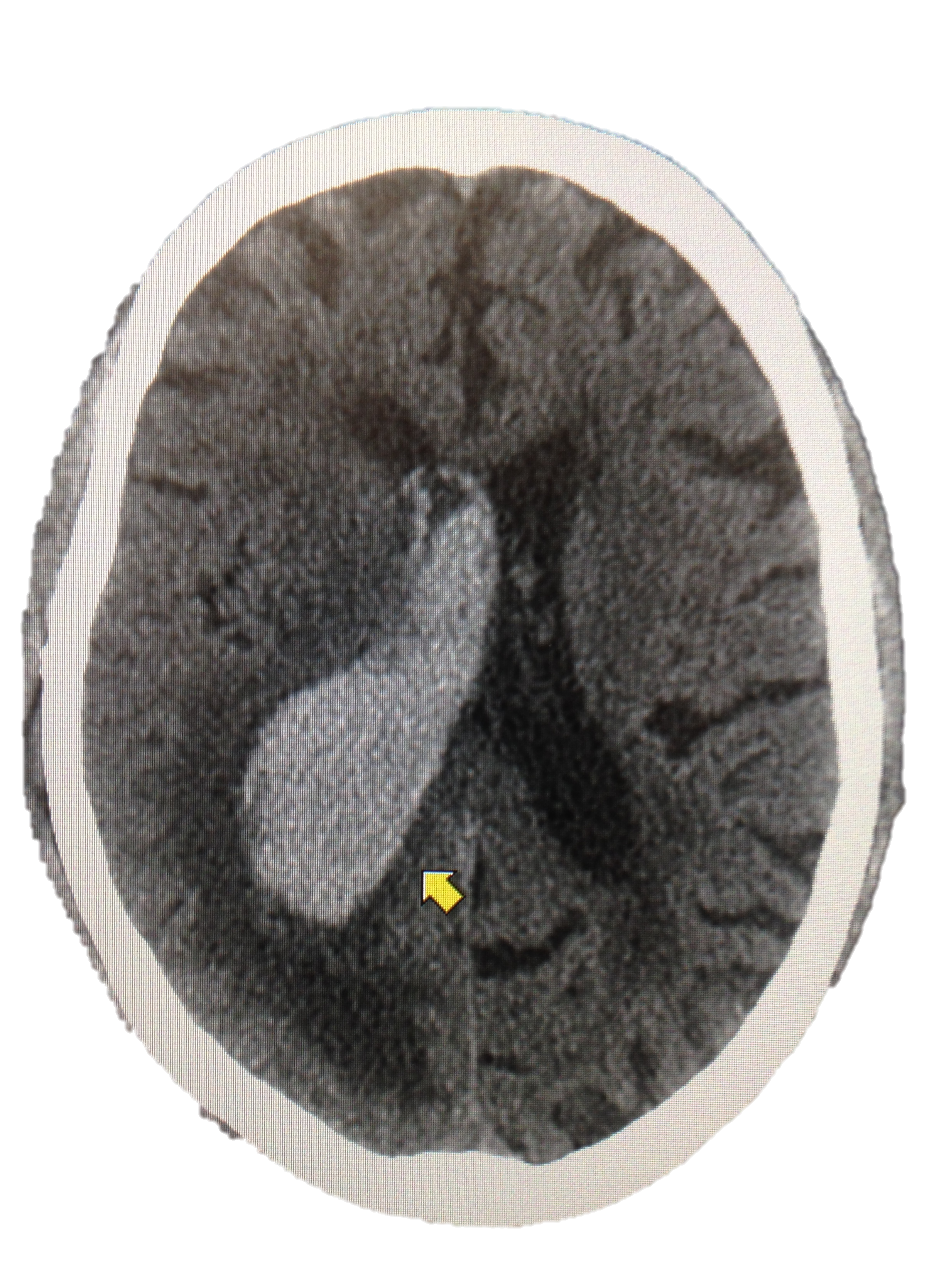
Image 5. Intraventricular hemorrhage without midline shift in patient on Novel Oral Anticoagulant (NOAC) after MVA Photo courtesy of the editor, Dr. Ruggero for educational purposes only with prior permission.
Diffuse Axonal Injury
Diffuse axonal injury results from shearing forces on axonal fibers of the white matter and brainstem. The mechanism of injury is typically a sudden deceleration, such as from a motor vehicle collision. Initial CT scans may be read as negative, although classically display punctate hemorrhages along the gray-white junction of the cerebral cortex and in deep structures of the brain. Edema can develop rapidly requiring prompt intervention. Prognosis can be devastating, often with permanent deficits if the initial injury is survived.
Skull Fractures
Patients with head injury should be carefully assessed for signs of skull fracture. Any lacerations should be meticulously explored for underlying fractures. Signs of basilar skull fracture include CSF otorrhea or rhinorrhea, hemotympanum, periorbital (“raccoon eyes”), or retroauricular ecchymosis (Battle sign), deafness, or 7th nerve palsy. Fractures may be classified as linear, depressed, or comminuted. Any fractures with overlying lacerations are considered open and IV antibiotics should be given.
Increased Intracranial Pressure and Herniation
The cranium is an enclosed structure with a fixed volume, normally occupied by the brain parenchyma, CSF, and blood within the vessels and sinuses. Because there is no room for expansion of this space, if there is significant bleeding or edema within the cranium it results in an increase in the intracranial pressure (ICP). An increase in the ICP may result in decreased perfusion of the brain, causing hypoxemia and further exacerbating injury. The response to increasing ICP is termed the Cushing reflex, consisting of hypertension, bradycardia, and respiratory irregularity.
Increased ICP may also result in herniation of the brain parenchyma. Image 6 demonstrates different types of herniation with a description of each.
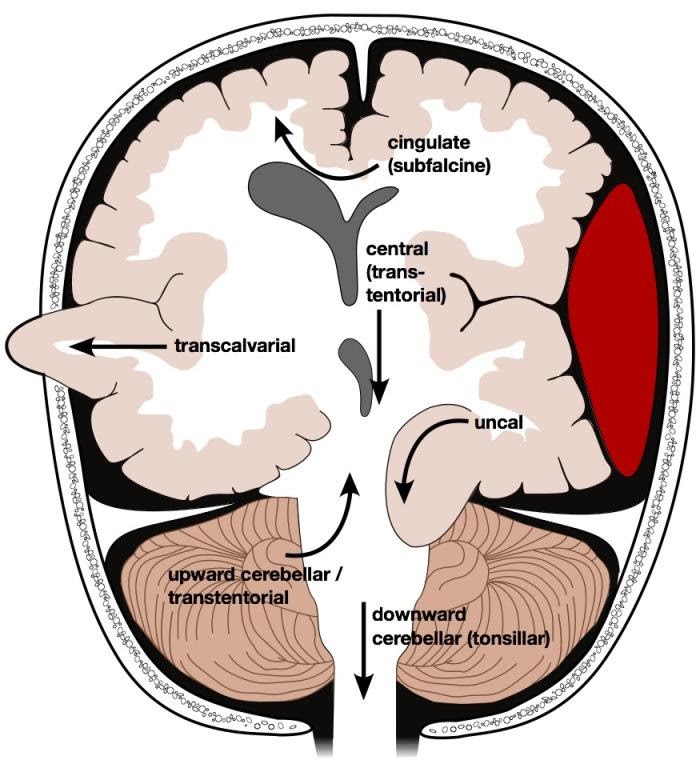
Image 6. Types of cerebral herniation. Image from WikiMedia Commons and used under the Creative Commons License.
Uncal herniation occurs when the uncus of the medial temporal lobe is displaced inferiorly through the tentorium. This results in an ipsilateral fixed and dilated pupil and contralateral motor paralysis.
Central transtentorial herniation occurs from midline lesions of the frontal or temporal lobes with downward displacement of the parenchyma through the tentorium. Clinical features include bilateral pinpoint pupils, bilateral Babinski’s signs, and increased muscle tone.
Cerebellotonsillar herniation occurs when the cerebellar tonsils are displaced through the foramen magnum, resulting in bilateral pinpoint pupils, flaccid paralysis, and sudden death.
Upwards transtentorial herniation results from posterior fossa lesions, consisting of conjugate downward gaze with lack of vertical eye movements and pinpoint pupils. Development of the Cushing reflex or a herniation syndrome requires prompt intervention to relieve intracranial pressure and prevent further injury.
Subfalcine herniation occurs with displacement of the cingulate gyrus under the falx cerebri. Often present with only a headache or asymptomatic.
Transcalvarial, also known as external herniation can occur with penetrating or severe injuries causing skull fractures.
Mild TBI and Concussion
Concussions are microscopic traumatic brain injuries that result in neurologic symptoms not related to an intracranial bleed. A mild TBI, also known as a concussion, is defined as a GCS score of 13-15 with associated signs or symptoms after a blunt force or acceleration-deceleration head injury. Signs and symptoms may include headache, vomiting, weakness, numbness, dizziness, decreased concentration, memory problems, sleep disturbance, irritability, fatigue, visual disturbances, depression, or anxiety. While there are no specific treatments, it is important to distinguish patients at risk for more serious injury that may require imaging and further intervention (further discussed in Diagnostic Testing section). Patients with negative imaging or in whom it has been determined that imaging is not necessary may be discharged, but require follow up with either their primary care doctor or TBI specialist if symptoms persist. Those patients should be advised to avoid sports or other activities that put them at risk for further head injury until medically cleared. A graded return-to-activity program is recommended before full resumption of normal activity. Repeat concussion during the vulnerable healing period following an initial concussion can result in second impact syndrome, with rapid onset of cerebral edema and death.
Diagnostic Testing
The main decision point in the assessment of a patient with head injury is whether or not to obtain a CT scan. All patients with head injury and a GCS less than 15, neurologic deficits, coagulopathy, or on anticoagulants should undergo a non-contrast CT scan of the head to assess for intracranial injury. For patients not meeting those criteria, two evidence-based decision rules, the New Orleans Criteria and the Canadian CT Head Rules, have been developed to further assess the need for CT scan (Table 2). Both sets of criteria have 100% sensitivity for detection of patients requiring neurosurgical intervention. Specificity of the New Orleans Criteria is 5%, while the Canadian CT Head Rules is 38%. The major difference in specificity between the rules is due to the New Orleans Criteria being developed to detect all patients with abnormality on CT, while Canadian CT Head rules account for only patients requiring intervention. As a result, sensitivity for detection of any intracranial abnormality approaches 100% for the New Orleans Criteria, while only 83% for the Canadian Head CT Rules.
Table 2. Comparisons of CT Head Decision Rules
Treatment
ABCs should be addressed as previously discussed. Depending on injury, clinical course may change rapidly, so frequent reassessment and appropriate intervention is crucial. Neurosurgical consultation should be obtained immediately in patients with pathology on CT scan or clinical signs of increased ICP or herniation. Emergent surgical decompression may be necessary to prevent impending herniation. If neurosurgery is not available at your center, arrangements should be made for rapid transfer to a trauma center.
Several temporizing bedside measures may be initiated to decrease ICP prior to definitive intervention:
- The head of the bed should be elevated to 30 degrees. If there is concern for spinal injury this may be accomplished via reverse Trendelenburg positioning.
- Mannitol may be used as an osmotic diuretic if the patient is not hypotensive, or hypertonic saline if hypotension is present.
- If there is concern for impending herniation a temporary course of hyperventilation may be instituted, with a goal PaCO2 of 30-35 mm Hg.
- Antiemetics if there is vomiting as vomiting increases the intracranial pressure.
- The patient may need to be intubated and adequately sedated to prevent agitation and increase in ICP. Seizures should be treated with benzodiazepines and IV antiepileptics.
In patients with coagulopathy found to have intracranial bleeding, reversal should be instituted immediately. This may include administration of vitamin K, fresh frozen plasma (FFP), prothrombin complex concentrate (PCC), four factor prothrombin complex concentrate, or other factors depending on your institutions policies.
Blood pressure management should focus on perfusion to the tissue, with goal CPP 60-70. There are data showing that maintaining SBP at ≥100 mm Hg for patients 50 to 69 years old or at ≥110 mm Hg or above for patients 15 to 49 or >70 years old may be considered to decrease mortality and improve outcomes.
Patients with intracranial injury on CT scan, persistently abnormal GCS, or persistent neurologic deficits, require admission to the hospital for further observation even if intervention is not immediately indicated. Those who do not meet admission criteria may be discharged home with a reliable companion who can observe them for at least 24 hours with proper care instructions and return precautions.
Pearls and Pitfalls
Maintain spinal precautions (c-collar, supine positioning) in all head injury patients until spinal injury can be excluded
When preparing to intubate, note a GCS, pupillary exam, and motor function in all extremities prior to sedating and paralyzing.
Patients with head injury require higher MAP goals (70-80 mm Hg) than typical trauma patients.
Watch for signs of increased ICP or herniation, including Cushing’s reflex (hypertension, bradycardia, irregular breathing), abnormal pupillary exam, or abnormal motor exam. Treat with elevation of the head of the bed, mannitol or hypertonic saline, controlled hyperventilation, and emergent neurosurgical consultation.
The elderly, chronic alcoholics, and those with coagulopathies or on anticoagulants are at high risk for significant injury from seemingly minor mechanisms – have a low threshold for imaging in these patients.
Reverse coagulopathy emergently if intracranial bleeding is revealed by imaging.
Negative imaging and a normal exam does not exclude injury. Patients with concussions should be given proper care and follow up instructions prior to discharge.
Case Study
In assessing your patient with headache after a fall, you established that her ABCs are intact. GCS is 13 (Eye 3, Verbal 4, Motor 6). Given her GCS of 13 and episodes of vomiting, she should receive imaging via either clinical decision rule for head injury. A CT scan of the head is completed which confirms a diagnosis of subdural hemorrhage with no midline shift. She is not on anticoagulation, and her vital signs remain stable. She is admitted for further evaluation and neurologic reassessments. Her neurologic symptoms gradually improve. Repeat head CT in 24 hours reveals no increase in size of her small subdural hematoma. She ultimately does well and is subsequently discharged with no permanent disability.
References
ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013 May;74(5):1363-6.
Barbosa et al. Evaluation and management of mild traumatic brain injury: An Eastern Association for the Surgery of Trauma practice management guideline. Journal of Trauma and Acute Care Surgery: November 2012 - Volume 73 - Issue 5 - p S307–S314. https://www.east.org/education/practice-management-guidelines/traumatic-brain-injury-mild
Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
EARLY INDICATORS OF PROGNOSIS IN SEVERE TRAUMATIC BRAIN INJURY https://www.braintrauma.org/uploads/01/03/prognosis_guidelines.pdf
Emergency Medicine: A Comprehensive Study Guide, 7th ed, Chapter 254, “Head Trauma in Adults and Children”, DW Wright and LH Merck.
