Approach to the Undifferentiated Patient
Author Credentials
Author: Gregory Tudor, MD, University of Illinois College of Medicine at Peoria
Update Author: Zachary Holt, MD, Wright State University; Stacey Poznanski, DO, Wright State University
Update Editor: Morgan D. Wilbanks, MD
Section Editor: Matthew Tews, DO, Indiana University School of Medicine
Last Updated: 2023
Objectives
By the end of this module, the student will be able to:
- List the steps in the approach to the undifferentiated patient in the ED.
- Describe the importance of the life threatening differential diagnosis in the ED.
- Classify the components of the primary and secondary ED survey.
- Utilize the concepts of pre-test probabilities and diagnostic testing in the ED.
Case Study
The case study for this chapter is used in a stepwise fashion to demonstrate the evaluation of a patient. It will be presented and resolved throughout the chapter.
Introduction
Patients presenting to the emergency department (ED) differ from those in other outpatient and inpatient settings. They are usually unfamiliar to the provider and believe they need urgent medical attention for what is perceived to be either an emergent condition or a medical need that they are unable to have addressed elsewhere. Emergency physicians function under the constraints of limited time, limited resources, and a seemingly endless line of patients waiting to be seen. As a result, the approach to the undifferentiated patient in the ED differs from other classic approaches in inpatient and outpatient settings, such as clinics or private practice offices. See table 1, Comparison of the Three Patient Care Settings. (Ref. 1)
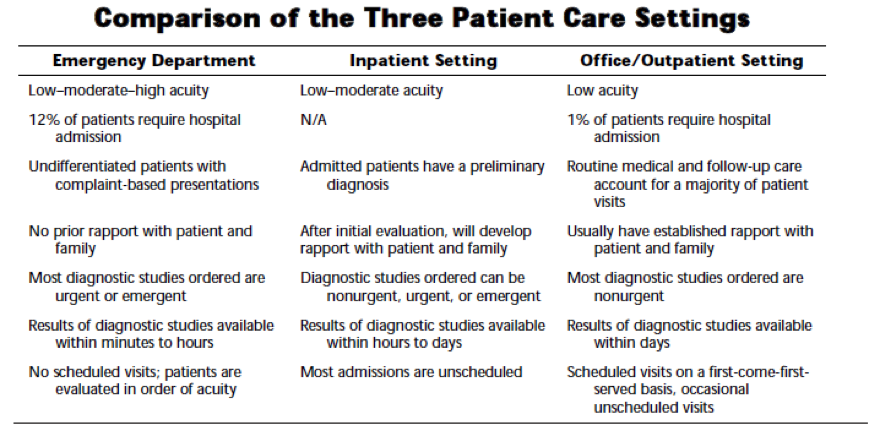
Table 1. Reproduced with permission from Wald D et al. Emergency Medicine Clerkship Primer: A Manual for Medical Students. Clerkship Directors in Emergency Medicine: 2008.
The first contact the patient will have with medical personnel in the ED is often a triage nurse, if time and patient condition allow. The patient’s chief complaint (CC), vital signs (VS), past medical history (PMH), past surgical history (PSH), medication list, allergies, and brief history of present illness (HPI) are recorded. It is often the decision of the triage nurse if the patient will return to the waiting room or be brought back for immediate evaluation. (Ref. 2) Many patients are stratified, or ‘triaged’, on a scale reflecting acuity and resource needs. The most common triage coding system, known as the Emergency Severity Index (ESI), was developed by Richard Wuerz and David Eitel in 1998 and contains five triage categories; Red (1) – Critical, Orange (2) – Emergent, Yellow (3) – Urgent, Green (4) – Minor, Blue (5) – Very minor. (Ref. 3)
When ED physicians assign themselves to a new patient, they review the information from triage, and begin the approach to the undifferentiated patient in the ED. The steps in this approach follow. We will use a classic example of a patient with “abdominal pain.”
Our patient:
CC: 69 year old female sent in by an outlying urgent care for right upper quadrant abdominal pain. (Patient was seen and evaluated by a physician; concern for gallbladder disease prompted the physician to advise the patient to seek care in the ED).
VS: BP 160/90 P 76 R 20 T 99.6 O2 99%
Significant PMH: Hypertension (HTN), Diabetes Mellitus Type 2 (DM), Hypercholesterolemia
Step 1. Initial Actions and Primary Survey
Review the triage note and see the patient.
Does the patient appear to be unstable or in any distress? Determine this with a basic assessment of the ‘ABCDEs’ (Airway, Breathing, Circulation,Disability, Exposure). This is a critical step in the determination of this patient’s degree of illness. It should take less than 60 seconds. If a problem with any of these is discovered, it should be addressed before proceeding to the next step:
A – Is the patient able to speak? Is their voice normal, muffled, high-pitched? Is there any obvious swelling to their face, mouth, or oropharynx? Are they displaying signs of imminent airway compromise (e.g. hands around their throat)?
B – Is their breathing pattern rapid or too slow? Are they grunting or audibly wheezing, or do you hear stridor? Are they displaying any other abnormal breathing pattern?
C – FEEL the patient’s pulse while directing someone to place the patient on the monitor. Can you palpate a radial pulse? If not, can you palpate a carotid? Is it fast or slow, regular or irregular? Other indicators of circulatory status are skin color (e.g. mottled) and blood pressure. This is also a good time to assess the status of vascular access so that IV fluid resuscitation can be initiated if indicated. Does the patient have a large-bore IV? Do you need to place an intraosseous (IO) line for rapid access?
D - Are they able to give a chief complaint, history or any other information (i.e. have a normal mental status)? AVPU assessment - Alert, Verbal - respond to voice, Painful - respond only to painful stimulus, Unresponsive; Do they have any obvious facial asymmetry? Are they able to move all of their extremities?
E - Completely undress the patient, looking under all splints, clothing, socks/shoes, wraps, back, buttocks, medication patches - entire skin assessment
For further discussion on unresponsive, pulseless, or otherwise critically ill patients, you can read Stabilization of the Acutely Ill Patient.
Next, a quick history should be obtained while help from other ED support staff is coordinated (resources may include: additional nursing staff, crash cart, respiratory therapy, physician back-up in educational settings). AMPLE is a useful mnemonic:
- A – Allergies: What is this patient allergic to?
- M – Medications: What medications is this patient taking?
- P – Past History: What are the pertinent medical/surgical conditions of this patient?
- L – Last Meal: When did this patient eat or drink last?
- E – Events: What are the brief events that led to this patient’s condition?
Are any immediate actions necessary?
The next question to ask is: are any immediate interventions required as a result of the findings during the initial impression and primary survey, such as IV fluids for significant hypotension, oxygenation for hypoxia, hemostasis for hemorrhage, glucose or naloxone for altered mental status, etc. If so, those actions must be completed first, before moving on to other steps. This is also a time to consider providing your patient with pain and/or fever control as indicated. Be sure to verify allergies first!
Based upon the initial impression, an important question should be answered: Is this patient “sick” (unstable, in imminent medical danger) or “not sick”? While discerning between the two is a skill that is developed with experience, clues include severe alteration of vital signs, general appearance (e.g. diaphoretic, pale, altered, etc.), or any abnormalities identified on the primary survey that would necessitate immediate action. It is important to recognize that patients may have a lethal diagnosis and not appear “sick” on presentation.
Once the competent emergency physician deems a patient “sick”, the following events should always occur, regardless of the cause: intravenous or other vascular access should be established and a cardiac monitor should be applied to the patient. Oxygen should be supplemented as needed. To remember these actions, think “IV-O2-Monitor”. Vital signs are vital and should be obtained as soon as possible. Recognize that for a “sick” patient, the steps delineated above (ABCDEs, IV-O2-Monitor, and AMPLE history) are steps that should be done in parallel, not in series. Most other interactions in medicine are performed in series (e.g. Chief Complaint, HPI, Medical History, Family History, Meds, Allergies, Physical Exam). In the “sick” patient, history, diagnostics, physical exam, and treatment are being done nearly simultaneously.
Our patient is alert, speaking clearly, and in no respiratory distress. She has a strong, regular pulse. She appears uncomfortable, but stable. At this time, she does not meet the “sick” classification. She denies any allergies and you order 75 micrograms of fentanyl IV to address her pain.
Step 2. Initial Differential Diagnosis – Focus on the Life Threats
Once the triage note has been reviewed and the initial assessment of the patient is complete, a list of possible diagnoses that are life or limb threatening to the patient should be formulated. This is initiated with the chief complaint and primary survey and refined after gathering more information. In an elderly female with right upper quadrant abdominal pain, like our patient, the classic life threats include both abdominal and cardiovascular emergencies. This differential would change slightly in a younger patient or with pain in the lower abdomen.
Abdominal aortic aneurysm (AAA)
Mesenteric ischemia
Acute coronary syndrome (ACS)
Bowel obstruction
Perforated viscus (e.g. ulcer)
Surgical biliary disease (e.g. cholecystitis or cholangitis)
Acute GI bleedAppendicitis
Appendicitis
Initial Differential Diagnosis for our patient:
Since our patient was initially deemed “not sick”, we can proceed to the Secondary Survey.
Step 3. Secondary Survey
The secondary survey includes a focused history and physical exam.
Focused History
If possible, give the patient two uninterrupted minutes to tell you why they sought medical care. You may be surprised by how often they tell you what you need to know. If, after a couple of minutes, they need some redirection with further questioning, it may be appropriate to redirect their history with specific questions.
The mnemonic COLD READ is helpful when obtaining a focused history:
- Character
- Onset
- Location
- Duration
- Radiation
- Exacerbating/Alleviating factors
- Associated symptoms
Different today – What has changed in the patient’s symptoms or presentation that prompted the current visit? This is particularly important in the ED and allows the physician to focus on why the patient decided to seek care today, a question not usually needed in the office or inpatient setting.
Next, ask specific questions that will ascertain any “pertinent positives and negatives” related to your differential diagnosis. This is information that will make a diagnosis more or less likely. Examples:
- Have you been sick to your stomach or sweaty?
- Have you ever had a blood clot in your legs or lungs?
- Have you traveled recently?
- Do you know anyone sick with similar symptoms?
- Have you been vomiting or had a fever?
Our patient: “I have had several episodes of pain in my stomach (points to right upper quadrant) over the past day. It began 2 days ago after we ate Chinese food at our local restaurant. It comes and goes, but this morning it was much worse. We went to the urgent care by our home. The doctor checked me over and said we needed to come here for a gallbladder test. I have these papers from his office.”
Patient hands you a brief note from the office: “Patient with right upper quadrant pain, negative Murphy’s but multiple risk factors. Normal exam, fecal occult blood negative stool, urine dip negative, ECG normal sinus, no STEMI, abdominal plain film negative for free air. Sent to ED for further evaluation.”
It is important to note that when a patient arrives from any outside facility (e.g. office, another ED) it is still essential to approach them as if they are undifferentiated. Starting with someone else’s diagnosis has potential danger and can lead to anchoring bias. Trust but verify.
Further history on the patient:
Character is a dull ache; Onset is 2 days ago; Location is right upper quadrant; Duration is episodic, worse this morning, several periods of pain resolution; Radiation is to epigastric area; Exacerbating factors are unclear – started after eating Chinese food 2 days earlier, unsure if related to food since (seemed to neither help nor worsen); Alleviating factors also unclear – took over the counter antacids which may have helped, nothing seems to have worked consistently; Associated Symptoms include nausea. Different today: pain worsened to 6/10, associated with nausea. Pertinent negatives include no recent travel or sick contacts.
The next component of an ED history is a focused Review of Systems (ROS). This is an important step to help discover other pathology that may be relevant or contributing to the patient’s disease process.
Our patient: ROS is positive for nausea; negative for vomiting or diarrhea; feeling generally more tired past 2 days; no ENT complaints, no ocular complaints, no fever/chills, cough or cold symptoms; no chest pain; no shortness of breath; no black or bloody stools; no urinary symptoms; no vaginal bleeding or discharge; no trauma; all other ROS negative.
Past medical, surgical, social and family histories, as well as medications, and allergies are important for this section and should be reviewed with the patient. Remember, not all information in an electronic medical record is accurate or up to date.
These items are still crucial to obtaining a thorough history.
Our patient:
- Medical History: DM (diet controlled), HTN, and hypercholesterolemia
- Surgical History: Hysterectomy 15 years prior for dysfunctional uterine bleeding
- Social History: Smoker – one pack per day for past 30 years, social alcohol only on weekends, denies drugs, married for 30 years, 2 grown children
- Family History: patient was adopted
- Home Medications: anti-hypertensive and cholesterol lowering agent (cannot recall names), occasional over the counter antacid
- Allergies: none.
Focused Physical Exam
Depending upon the chief complaint and urgency of the patient’s clinical condition, the physical exam can be adapted or focused. With every patient encounter, the physical exam should be as complete as possible. This is especially true in the patient presenting with altered mental status. Always start by noting the vital signs and a general appearance.
In our patient with abdominal pain, we can proceed with a full, but expeditious physical exam:
VS: unchanged from above
Gen: Mildly obese female appearing stated age holding her right upper quadrant in moderate distress.
HEENT: No scleral icterus, no facial asymmetry, no other abnormalities
Neck: No masses, no JVD, supple and non-tender
CV: Regular rate and rhythm, no murmurs, rubs or gallops; distal pulses 2 plus and equal
Lungs: Clear to auscultation, no respiratory distress
Abdomen: Normal inspection – no rash or bruising; normal bowel sounds; no hepatosplenomegaly, no masses, no rebound, no abdominal tenderness to palpation – specifically no tenderness at the right upper quadrant where the patient localizes her pain; Negative Murphy’s sign.
Rectal: normal tone, fecal occult blood negative
GU: patient declined exam
Extremities: warm and well-perfused, non-tender, no edema
Neurological: Alert and Oriented, mental status appears intact; moving all extremities equally and without obvious deficit; speaks clearly; no facial droop or asymmetry
Step 4. Refine the Differential Diagnosis
Once more information on the patient has been collected in the above manner, the differential list can be refined. Diagnoses that are common, but not necessarily imminently life threatening, can be included such as the following for a patient with RUQ abdominal pain: pancreatitis, gastric mucosal disease (gastro-esophageal reflux, ulcer, etc), bowel ileus, occult trauma, hepatitis, urinary tract infection, kidney stone, hernia, gynecologic pathology, and herpes zoster.. In addition, you can remove items from the initial list felt to be less likely, as dictated by the findings thus far.
The differential for our patient at this point would likely still include: AAA, mesenteric ischemia, acute coronary syndrome (ACS), biliary colic from gallstones, gastro-esophageal reflux, ulcer, hepatitis, and a kidney stone.
Diagnoses that are becoming less likely based upon exam (especially her abdominal exam) and history are: bowel obstruction, perforated viscus (e.g. ulcer), acute GI bleed, surgical biliary disease, appendicitis, hernia, urinary tract infection, occult trauma, herpes zoster, gynecologic pathology.
Step 5. Diagnostic Testing
With your differential diagnosis in mind, it is important to pursue a diagnostic strategy that rules out life-threatening disease (when possible) and rules in more likely or more common disease (when possible). The tests you decide to order should be based upon pretest probabilities you have assigned, and any clinical decision tools being utilized (further discussion of these topics follows the case). It is extremely important to know what you will do with the results of any test you order and how they will affect management and disposition. You should only order tests to help confirm or rule out diagnoses on your differential. DO NOT order tests to form your differential. When ordering tests, especially those that are common in the ED, you should have a plan in place for any pertinent results and be prepared to make appropriate interventions. Consider cost, time, and potential harm to the patient (e.g. radiation exposure) in this step.
For our patient, several tests will play an important role in the work up, management, and disposition. A complete blood count, comprehensive metabolic panel, lipase, urinalysis, lactate, ECG, abdominal ultrasound, and possibly a CT seem to address our differential diagnosis. Are there other tests you would consider at this point in the patient’s evaluation?
Prior to the results of any tests becoming available, the nurse informs you that the patient is now ready to be taken to ultrasonography for a formal right upper quadrant ultrasound. The patient is complaining of increased pain and is requesting pain medication. The patient received your initial order of 75 micrograms of fentanyl IV 30 minutes ago, however the patient is now complaining of increased pain and is requesting additional pain medication:
Your choices:
- Send the patient to the ultrasound suite to obtain her scan.
- Re-dose the medication and then send the patient to ultrasound.
- Cancel the ultrasound and obtain a surgery consult (you will have to explain this to the surgeon).
- Obtain a CT of the abdomen.
- Wait for the other results and then choose one of the above (this will take about 30-40 more minutes).
- Re-evaluate the patient.
Step 6. Patient Re-Evaluation
Emergency medicine (EM) occurs in a dynamic environment with patient’s illnesses often manifesting, progressing and changing while they are in the ED.
Whenever there is a change in the condition of the patient (such as increasing or resolved pain, development of new symptoms, or a change in mental status or vital signs), the patient should always be re-evaluated and your differential diagnosis revisited. Has
the patient gone from “not sick” to “sick”?
Re-evaluation of our patient:
Repeat vitals VS: BP 170/84 P 56 R 24 T 99 O2 99%
General: Patient is now diaphoretic, clutching her right upper quadrant, tearful despite the pain medication, and asking for you to help her
CV: Now bradycardic, distal pulses intact, no murmurs, rubs or gallops
Lungs: Clear, unchanged
Abdomen: Essentially unchanged: Soft, normal bowel sounds, no masses, femoral pulses intact and equal, no tenderness, specifically no tenderness elicited on exam of right upper quadrant, however patient continues to localize her pain there.
Skin: Now diaphoretic
Extremities: Warm and well-perfused
We should now revisit our differential diagnosis: AAA, mesenteric ischemia, acute coronary syndrome (ACS), biliary colic from gallstones, gastro-esophageal reflux, ulcer, hepatitis, and kidney stone. The most life threatening of these are AAA, mesenteric ischemia and ACS. The most likely of these with the new bradycardia, the more localized upper abdominal pain, and lack of hypotension (which may indicate a rupturing AAA) is ACS. This can be quickly addressed with a bedside ECG and this should become the priority. If that is negative for a STEMI, a bedside ultrasound to evaluate for a AAA would be the next best step. With the patient’s status changing, she has now entered into the “sick” category and you should act quickly and think twice before allowing the patient to leave the ED.
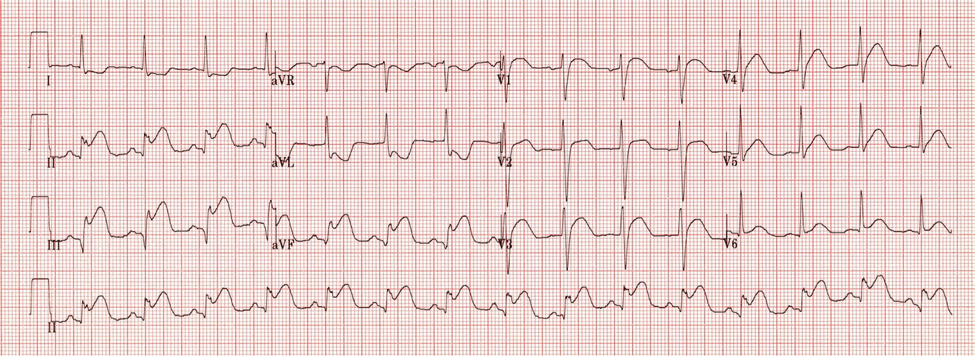
Her ECG:
Figure 1. The Patient’s EKG. Image courtesy of Life in the Fast Lane. Used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International license. Original Image located at: Inferior STEMI • LITFL • ECG Library Diagnosis.ECG Interpretation: Inferior STEMI (Marked ST elevation in II, III and aVF with early Q-wave formation; Reciprocal changes in aVL; ST elevation in lead III > II with reciprocal change present in lead I and ST elevation in V1-2 suggests RCA occlusion with associated RV infarction. (The patient could have right-sided leads to confirm this.) (Ref. 5)
As with any change in status or new information that provides critical results, an action should follow. What would you do now?
Call the cardiac catheterization lab for immediate intervention, give aspirin, and have the crash cart ready. Nitroglycerin should be avoided, as it may cause significant hypotension in patients with inferior MI. Now is a good time to cancel the sonogram as well.
Step 7. Treatment and Disposition
All active patients in the emergency department have one of three dispositions: they are admitted, transferred, or discharged (some EDs have clinical decision or observation units and that is a separate discussion altogether). The decision to admit, transfer, or discharge is an important one, especially with high risk complaints such as chest pain, headache, shortness of breath, abdominal pain, and altered mental status. Emergency physicians must always advocate for the patient and consider the risks and benefits of their actions. It is important to address the patient’s symptoms and treat the underlying causes, guided by the patient’s progression and the findings from the diagnostic workup.
Sometimes, deciding whether to admit a patient is easy, such as in those patients that are clearly “sick” and in need of acute medical or surgical attention. This was the case for the example patient, whose disposition was to an interventional cardiologist in the cardiac catheterization lab. This becomes more complicated if certain services are not available, and transfer of the patient is indicated. It is important to know ahead of time (e.g. when starting a new job, working overnight, working the holidays, etc.) what policies are in place and what resources are available on a shift in the ED.
When it is appropriate to discharge patients, several key things must be considered and conveyed:
- Summarize the findings and specific treatment plan for the patient. Answer any questions they may have using simple, non-technical language (as if speaking with a 4th grade student).
- Arrange appropriate and timely follow up with an outpatient provider. Contacting the patient’s primary physician to arrange a specific appointment time may improve compliance for follow up.
- Provide detailed instructions for reasons to return to the ED. Many electronic medical records, such as EPIC, have pre-written summaries and return precautions available that can be provided at the time of discharge. Ensure these provide accurate information in your patient’s current clinical situation.
Explain to the patient any additional instructions related to their presentation and treatment (e.g. continuing their current medications, use of over-the-counter medications as needed, any restrictions pertaining to activity or driving)
Step 8. Pearls and Pitfalls
- This patient presents with a history consistent with several abdominal etiologies, such as gallbladder disease, EXCEPT for a lack of tenderness when palpating her gallbladder or abdomen, which should prompt suspicion regarding biliary disease as a diagnosis. This patient has many risk factors for coronary artery disease (CAD). After undergoing successful percutaneous coronary intervention (PCI), stent placement and further inpatient treatment, the patient related further important history: “When I said my pain started after I ate Chinese food, it really did. What I didn’t get to tell you when you started asking questions was that it was 2 hours later and occurred as my husband and I were walking up a long pathway in the local park. I stopped and it seemed to get better, so we continued to walk and it happened again. We decided to turn around and go home.”
- This is a classic case of a common disease presenting in a less common way, and illustrates several important points about management of the undifferentiated patient.
- The best clinicians in EM will always look for dangerous diseases that present in atypical ways. Thus, it is critical to obtain a meticulous history if possible. The vast majority of the time, the diagnosis will be buried in the history, with the physical exam contributing confirmatory evidence.
- Sometimes, it is important to ask specific questions regarding exacerbating and alleviating factors in order to get complete information. After asking “Does anything make it better or worse?” consider adding “Is it worsened by food? Is it worsened by exertion or relieved with rest?”
- While it is important to review information obtained by other providers prior to your visit with the patient in the ED, it is crucial to avoid being biased by that information. The example patient was sent in for a “gallbladder evaluation.” ACS or other life threats could be easily missed if each item on your differential diagnosis is not addressed appropriately, either through history, physical exam, or diagnostic testing.
- It is important to remember the limitations of all diagnostic tests we use in the ED. Remember the urgent care ECG that reportedly did not show an ST elevation MI? Discover more in the last section.
Pre-Test Probabilities and Test Characteristics
An EM diagnosis often requires a combination of clinical gestalt, history and exam findings, vital signs, and knowledge of specific test characteristics and pretest probability. For the example patient, the chief complaint, history, and vital signs alone are likely to lead away from the correct diagnosis. ED physicians rely heavily on certain tests, and it is very important to understand their performance, reliability, and limitations. In addition, the results of those tests must be interpreted in light of the patient’s risk factors, the prevalence of disease in the surrounding population, and the pretest probability.
In the above example, the first ECG was obtained at an outlying facility. A review of that ECG yields the same interpretation given by the first physician who saw the patient: normal sinus rhythm, non-specific ST wave flattening, no acute injury pattern. An ECG is an example of a test that captures a moment in time; it is conceptually similar to comparing a photograph with a video clip. While a more accurate assessment of a patient’s cardiac status would be continuous 12 lead ST segment monitoring, this is not commonly available. Repeating ECGs over time, especially with changes in patient condition, can be an excellent way to evaluate evolving processes that were not evident at the initial presentation.
Next, we will discuss pretest probability and scoring systems. We will use the example of Well’s Criteria for pulmonary embolism (PE) (Ref. 6 & Ref. 7) Well’s Criteria is a clinical decision tool, or clinical prediction rule. A clinical decision tool is based upon medical research that attempts to identify a combination of signs, symptoms, and other findings to predict the probability of a disease or outcome. Many different clinical decision tools are available, and commonly used tools in the ED include PERC (Pulmonary Embolism Rule-Out Criteria) and many of the NEXUS criteria. Factors included in the Well’s Criteria clinical decision tool include the following, with the associated point value applied for each question answered “yes”:
- Clinical signs and symptoms of deep vein thrombosis (DVT) (3 points)
- PE is #1 diagnosis, or equally likely (3 points)
- HR > 100 bpm (1.5 points)
- Immobilization at least 3 days or Surgery in the previous 4 weeks (1.5 points)
- Previously, objectively diagnosed PE or DVT (1.5 points)
- Hemoptysis (1 point)
- Malignancy with treatment within 6 months or palliative care (1 point)
Scoring system and interpretation
- ≤4 = low risk group for pre-test probability of PE. A negative D-dimer may be an appropriate test for ruling out a PE.
- >4 =high risk groups for pre-test probability of PE. A D-dimer is not sufficient to rule out PE because the post-test probability is still too high, even with a negative test. Imaging is necessary to evaluate for PE.
Consider the example patient. If PE were in the differential, she would fall into the low risk group based upon the available information. Therefore, a negative D-dimer result would be sufficient to rule out the diagnosis and imaging would not be required. While there are limitations to every clinical decision rule, they can be helpful to help guide the workup in the ED, given the constraints discussed above.
MDCalc is one of many online resources where you can find this, and other, clinical decision rules, calculators, and evidence based medicine resources.
Conclusion
In the ED, patients often present with vague or misleading complaints. They come with a fear that something is acutely wrong, and it is the job of the emergency physician to evaluate for emergent diagnoses and improve patients’ current condition. This may be done with symptom control, reassurance, ensuring adequate follow-up, referral for definitive treatment, or admission. A genuine, caring approach is an important complement to the actual diagnostic and therapeutic accuracy of the physician. If there is concern that the patient may do poorly if discharged home, consider additional consultations in the ED or admission. Remember to think “worst first” when dealing with the undifferentiated patient in the ED, and always strive to do what is best for the patient. Keeping the life threats on the differential diagnosis, performing a thorough but timely history and physical examination, knowing the limitations of testing, and advocating for the patient’s best interest will yield high quality emergency care.
References and Suggested Reading
- Wald D et al. Emergency Medicine Clerkship Primer: A Manual for Medical Students. Lansing, MI: Clerkship Directors in Emergency Medicine: 2008. Electronic version available on the CDEM Web site.
- Hamilton G. Introduction to Emergency Medicine. In: Hamilton G et al. Emergency Medicine: An Approach to Clinical Problem Solving, Second Edition. Philadelphia, PA: W.B. Saunders Company; 2003: 3-16.
- Gilboy N, Tanabe T, Travers D, Rosenau AM. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook 2012 Edition. AHRQ Publication No. 12-0014. Rockville, MD. Agency for Healthcare Research and Quality. November 2011.
- Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. “Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care” Circulation 2010; 122(suppl 3) S729–S767.
- Burns, E. (n.d.). Inferior STEMI. Accessed on January 19, 2023, from https://litfl.com/inferior-stemi-ecg-library/
- Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83(3):416-20. PMID: 10744147.
- Wolf SJ et al. Prospective validation of Wells Criteria in the evaluation of patients with suspected
pulmonary embolism. Ann Emerg Med. 2004 Nov;44(5):503-10. PubMed PMID: 15520710. - Slovis B. Wells’ Criteria for Pulmonary Embolism calculator. MDCalc. Accessed on January 19, 2023. https://www.mdcalc.com/calc/115/wells-criteria-pulmonary-embolism