Introduction to Bedside Ultrasound
Author Credentials
Author: Matthew Lohse, MD, AEMUS FPD, Baylor Scott & White-Temple Medical Center
Update Author: Harry J. Goett, MD, Lewis Katz School of Medicine, Temple University
Editor: William Alley, MD, Wake Forest.
Section Editor: Navdeep Sekhon, MD, Baylor College of Medicine
Update: 2023
Case Study
It's a busy day in your ER when the following patient walks in:
A 55-year-old male presents to the emergency department after a syncopal episode. EMS noted that his on-scene vital signs were BP 90/60, HR 110, RR 20, satting 98%, and he is afebrile. His current VS are BP 110/70, HR 95. He complains of generalized abdominal pain but is nontender on exam. He has not seen a doctor in years, and has no known past medical history. His social history is positive for 30 pack-years of smoking. The patient’s 12-lead EKG performed in triage is normal. Labs are pending and CT of the abdomen/pelvis is going to take several hours to obtain due to a packed ED. You are concerned about your patient’s condition, what is your next action in this patient’s evaluation?
Objectives
By the end of this module, the student will be able to:
Understand the basic physics, knobology, and transducer orientation of ultrasound.
List the core ultrasound applications used at the bedside in the Emergency Department.
Recognize common pathologic findings detectable on core emergency ultrasound studies.
Introduction
Ultrasound has been used at the bedside in the emergency department (ED) since the 1980s to answer specific clinical questions and speed the diagnosis and treatment of patients. Over the last four decades, the use and applications of ultrasound in the ED have expanded to include:
Diagnostic evaluations
Therapeutic and resuscitative uses
Procedural guidance.
The Accreditation Council for Graduate Medical Education (ACGME) and all the major emergency medicine professional societies, including the American College of Emergency Physicians (ACEP), the Society for Academic Emergency Medicine (SAEM), and the American Academy of Emergency Medicine (AAEM), include ultrasound within the scope of practice of emergency medicine physicians and mandate it as part of emergency medicine residency training. An understanding of the use of ultrasound in the emergency department is therefore necessary for medical students planning on entering emergency medicine residency training.
Emergency ultrasound combines three traditionally distinct parts, all performed by the EM physician:
Obtaining the relevant ultrasound images
Interpreting those images
Applying this information to patient care.
By combining these elements which were traditionally performed by the ultrasound technician, the radiologist and the treating physician separately, the EM physician can speed the care and disposition of patients in the Emergency Department. Possessing good working knowledge of ultrasound and the technical skills to obtain and interpret images allows the treating physician to improve overall patient care by hastening time sensitive diagnoses, enhancing the safety of necessary procedures, and better adapting therapeutic strategies to individual patient physiology.
Physics
Far beyond the range of normal human hearing (20 Hz to 20,000 Hz), diagnostic ultrasound utilizes sound waves (energy) in the range of 2-18 MHz transmitted through the tissues of the human body to evaluate for disease processes and aid in therapeutic procedures. The piezoelectric effect is fundamental to creation of these waves via crystals in the transducers, or probes, of the ultrasound machines. The sound waves are produced by a current which is applied to the crystals, producing a vibration emitted as an ultrasonic wave. The transducer acts as both a speaker and a microphone which emits these waves and receives the returning waves after being reflected by tissue. The ultrasound computer then processes these returning waveforms to create an image on the screen that can be interpreted for diagnostic or procedural guidance purposes (Figure 1)
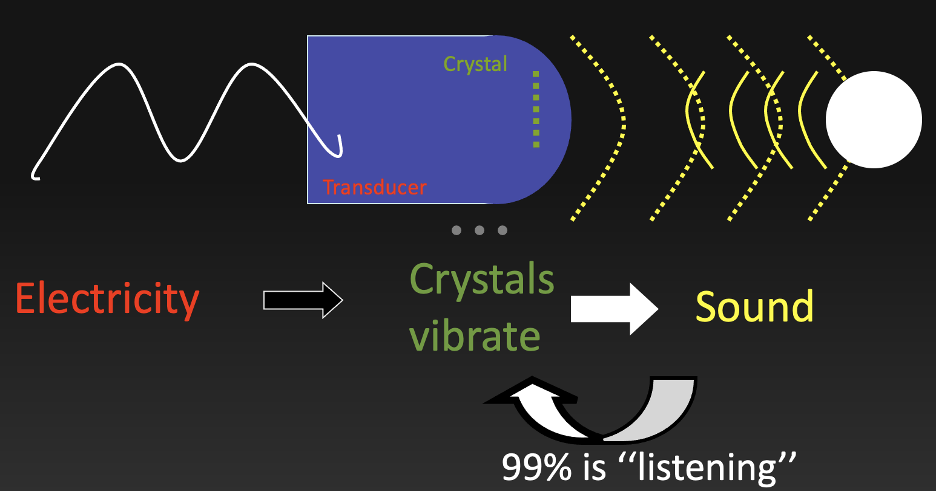
Figure 1. Ultrasound transducer components (Image courtesy of Matthew Lohse, MD. Baylor, Scott & White-Temple).
Many factors influence the velocity of ultrasound waves transmitted through the human body including tissue densities and tissue stiffness. A few key ultrasound physics concepts are explained below:
Density – the velocity of ultrasound waves traveling through tissue depends on the density of the tissue
Reflection – reflection occurs at interfaces between tissues of different densities
Refraction – the bending of sound waves at tissue interfaces as the ultrasound waves strike them obliquely
Scatter – reflection of ultrasound waves from tiny objects such as small areas of gas
Attenuation – the diminution, or weakening, of ultrasound wave energy as it passes through a medium
Frequency – this property of ultrasound waves determines image resolution and depth of tissue penetration. High frequency → high resolution, low depth of penetration
Artifact - incorrect representation of anatomic structure or motion due to a violation of basic assumptions of ultrasound physics, e.g. shadowing behind bone/gallstones
Equipment
Many manufacturers produce ultrasound machines (Figure 2), but they all have basic components in common: a transducer which transmits and receives the ultrasound signal, a central processing unit which interprets the signal, a control panel with buttons or simply a touch screen which has become more popular in recent years for its ease of cleaning, and a display screen which projects the images produced.

Figure 2- Common cart-based ultrasound machines with multiple transducer ports (Image courtesy of Matthew Lohse, MD. Baylor, Scott & White-Temple).
Transducers
Ultrasound transducers come in many shapes and sizes designed for various applications. Common configurations include curvilinear, linear, phased array and endocavitary transducers, among others.

Figure 3 - Curvilinear transducer (Image courtesy of Matthew Lohse, MD. Baylor, Scott & White-Temple).
Curvilinear - The image above demonstrates a larger curved “footprint” transducer that is typically used for abdominal, obstetrics, and gynecology imaging (Figure 3). Curvilinear transducers transmit ultrasound waves in the range of 1-5 MHz which allows for imaging of deeper structures at the expense of resolution.

Figure 4 - Linear array transducer (Image courtesy of REBELEM. Used under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. Original image located at: 10-6MHz-38-mm-Linear-Array-Probe-Ultrasound-Accessory - REBEL EM - Emergency Medicine Blog.
Linear array - This transducer (Figure 4) has a flat face and is typically used for vascular, musculoskeletal, nerve, ocular, and small-parts imaging. It transmits ultrasound waves in the range of 4-15 MHz allowing for higher resolution imaging of superficial structures.
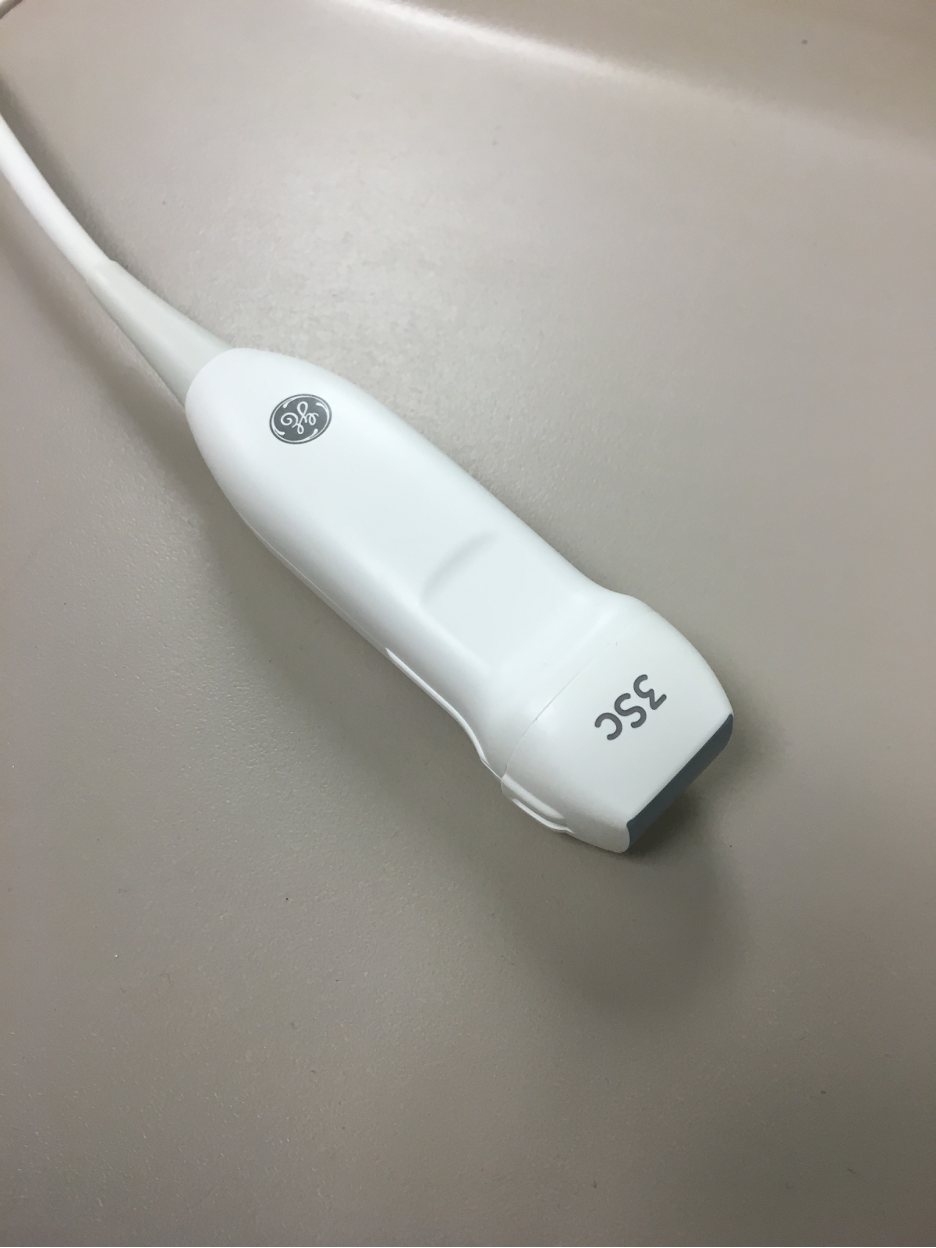
Figure 5 - Phased array transducer (Image courtesy of prior version of chapter).
Phased-array/Cardiac – Phased-array transducers (Figure 5) have a small flat footprint that facilitates intercostal imaging of the heart, although they can be used for many applications. They are used with a high frame rate setting to yield higher temporal resolution of a moving structure, i.e. the beating heart. They have a small superficial field of view which can limit superficial imaging and transmit in the frequency range of 1-5 MHz.
Endocavitary – Endocavitary transducers (Figure 6) are small-footprint curved-array transducers that can be inserted into an orifice to obtain imaging closer to the structure of interest. They are typically placed endovaginally to obtain gynecologic and obstetric images but are also used to visualize peritonsillar abscesses among other applications and transmit in the frequency of 5-9 MHz.

Figure 6 - Endocavitary transducer (Image courtesy of prior version of this chapter.)
Ultrasound Gel and Covers
To decrease the amount of air between the patient and the ultrasound probe, ultrasound gel is used between the ultrasound transducer and the skin. Because ultrasound waves are poorly transmitted through air, the gel provides a medium with similar impedance to human tissue that the ultrasound waves can easily pass through.
Various types of probe covers (Figure 7) are available for infection prevention when performing diagnostic ultrasound, such as endovaginal ultrasound, and to maintain sterility during ultrasound guided procedures such as central venous catheter placement.

Figure 7 - Sterile transducer cover. (Image courtesy of prior version of this chapter).
Knobology and Probe Orientation
With a little experience, a sonographer should be able to obtain quality images on any machine, regardless of the number of knobs on the control panel, by manipulation of a few standard settings.
Depth
Visualized on the right hand-side of the display screen, calibrated in centimeters, the depth of the image can be adjusted up or down using buttons or a knob to ensure adequate visualization of the structure or region of interest (Figure 8).

Figure 8 - Depth of tissue being imaged (cm) is denoted by right-side scale (Image courtesy of Matthew Lohse, MD. Baylor, Scott & White-Temple).
Gain
Gain can also be manipulated using slides or knobs on the control panel and adjusts the brightness of the image such that dark, hypoechoic tissue, such as blood or urine, appears black, and bright, hyperechoic tissue, like bone, appears white (Figure 9). Gain can also be selectively adjusted in the near and far areas of the image using time gain compensation.
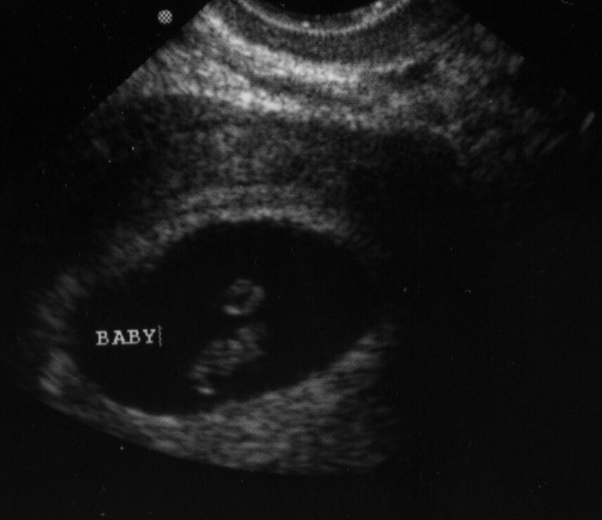 |  |
Figure 9 - Gain adjustment: the gain in the left image is too low and therefore dark ("ultrasound-20060914" by Jim Nutt is licensed under CC BY-NC-SA 2.0.), while the gain is too high on the right image and is therefore overly bright ("Baby McBride Ultrasound 6 Weeks 3 Days" by Nogwater is licensed under CC BY-SA 2.0)
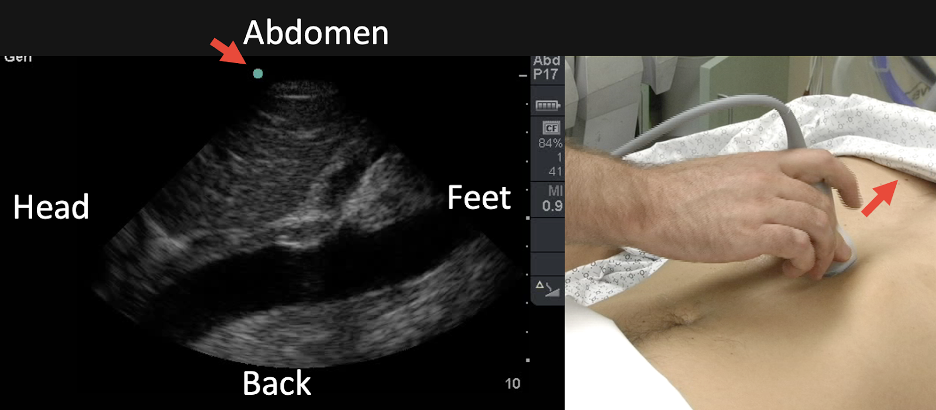
Probe Orientation
Maintaining transducer/probe orientation while scanning is essential to yield images that are understandable in their anatomic context. Each US probe has a groove or raised nub of plastic on one side of its long axis, as demonstrated in Figure 10 below.

Figure 10 Example of transducer marker ("Transducer marker" by iem-student.org is licensed under CC BY-NC-SA 2.0.)
Next, it is important to take note of the display screen marker, denoted by a dot or manufacturer icon adjacent to either the upper-left or upper-right corner of the image. For most emergency ultrasound imaging conventions, the upper-left corner
is standard. By maintaining ipsilateral alignment of probe marker and screen marker, the image will be oriented as in Figure 11 below for each standard anatomic view plane.
 a
a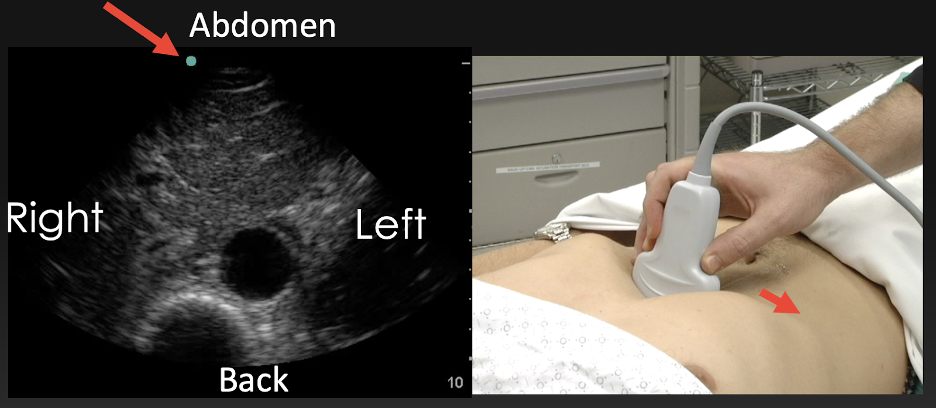 b
b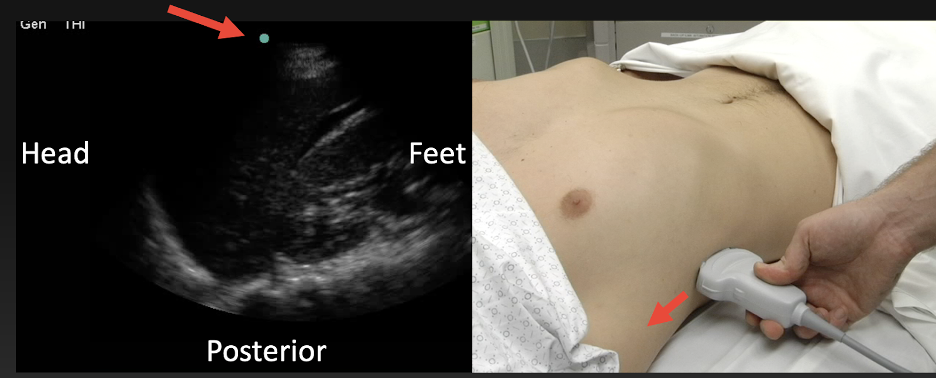
Figure 11 Imaging the abdominal aorta in a) long-axis sagittal plane b) short -axis transverse/axial plane, and c) right upper quadrant Morison’s pouch view in coronal plane. Red arrows indicate probe and screen marker (Image courtesy of Matthew Lohse, MD. Baylor, Scott & White-Temple).
Ultrasound Modes
B-mode – Displays a two-dimensional gray scale ultrasound image of anatomic structures and tissues, known as the “home” mode for ultrasound imaging (Figure 12).
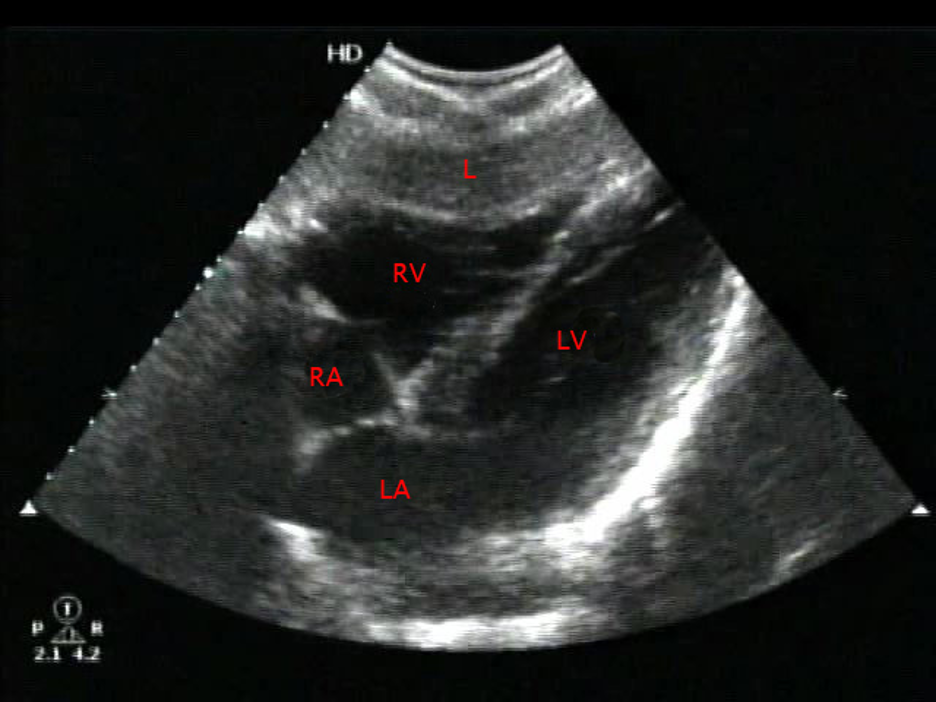
Figure 12 - B-mode image of the heart from a subxiphoid window. Courtesy of emDOCS and used under the Creative Commons Attribution 4.0 International License. Original image located at: emDOCs.net – Emergency Medicine EducationCore EM: Ultrasound Guided Pericardiocentesis - emDOCs.net - Emergency Medicine Education
M-mode – Displays a single plane of anatomic information graphed over time in the x-axis (Figure 13). This is a historical mode employed in early echocardiography but retains utility in modern ultrasound practice
for its high temporospatial resolution characteristics, allowing precise measurements of distances between moving structures, frequently in the heart but also for measuring collapse/expansion of vascular structures such as the inferior vena cava.
The M-mode can also be helpful in calculating the heart rate of a fetus.
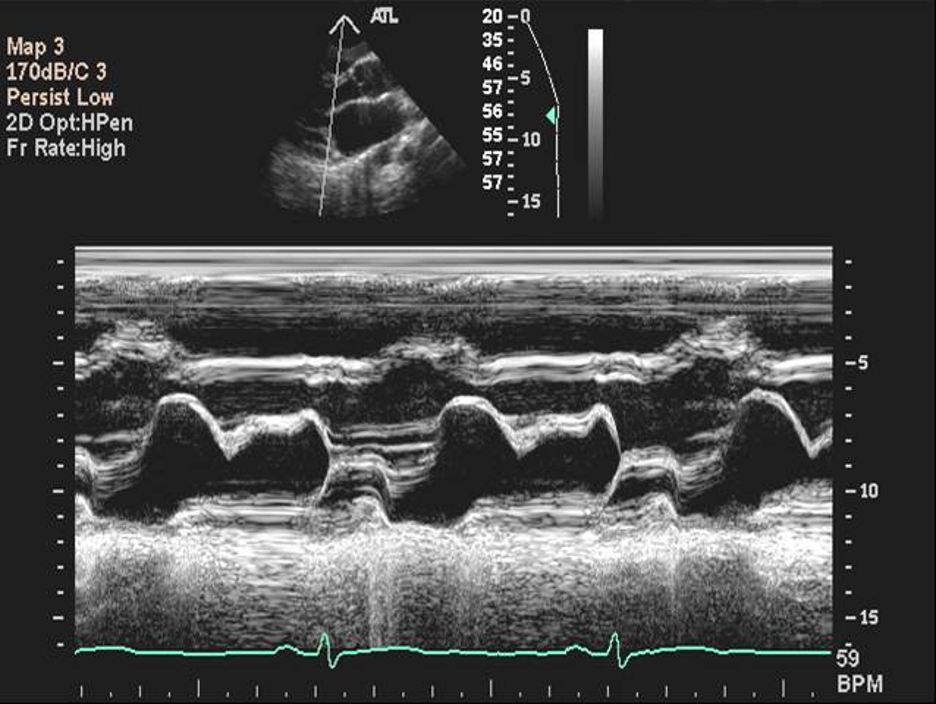
Figure 13 - M-mode tracing of the heart from parasternal long axis window demonstrating mitral valve movement over time. B-mode scout image at the top shows the adjustable white line localizing the anatomical plane being viewed. Image courtesy of Wikidoc and used under the Creative Commons Attribution/Share-Alike License. Original image is located at: M-mode echo: principles and classic findings - wikidoc.
Spectral Doppler – This mode employs the Doppler principle by detecting frequency shifts of a moving medium and is mainly used to detect blood flow, displayed as velocity and direction of flow (Figure 14). Common
applications include advanced assessments of cardiac valvular pathology, systolic and diastolic function, and vascular stenosis. It is available in pulse and continuous wave settings, depending on the range of velocities being evaluated.

Figure 14 - Pulse wave Doppler tracing of carotid arterial blood flow. Image courtesy of Daniel W. Rickey. Used under the CC-BY-SA 2.5 license. Original image located at: SpectralDopplerA - Doppler ultrasonography - Wikipedia.
Color Doppler – Displays Doppler signal with color scale superimposed on 2D image, where the convention is blue denotes flow away from the transducer and red denotes flow toward the transducer (Figure 15a).
Power Doppler - Power Doppler is not flow direction-dependent and is especially useful for assessing small blood vessels and ducts/vessels with low-velocity flow, such as ureteral jets into the bladder (Figure 15b).

Figure 15a - Color Doppler flow of a testis. Image courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Original image located at: Ultrasound Case 065 • LITFL • POCUS Self-Assessment Quiz.

Figure 15b. Power Doppler of the testis. Image courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Original image located at: Ultrasound Case 065 • LITFL • POCUS Self-Assessment Quiz.
Core Emergency Ultrasound Applications
In 2016 the American College of Emergency Physicians (ACEP) updated their 2008 policy statement on the use of ultrasound in the emergency department, listing 12 core emergency ultrasound applications.(5)
Trauma
The focused assessment with sonography for trauma examination, or FAST examination, is used in the setting of trauma to evaluate for free fluid in the abdominal cavity due to vascular, solid organ, or hollow viscus injury.
The standard views in the FAST examination include the:
subxiphoid/subcostal 4-chamber heart view (Figure 16)- to assess for pericardial effusion and tamponade
right-upper quadrant abdominal view to visualize the potential space between the liver and the right kidney, known as Morison’s pouch (Figure 17)
Left-upper quadrant abdominal view to visualize the space between the spleen and the left kidney (splenorenal interface), as well as the subphrenic space above the spleen (Figure 18)
Pelvic transverse and sagittal view (Figure 19) to evaluate for free fluid in the pelvis in the dependent rectovesical space in men and the rectouterine space in women (pouch of Douglas).

Figure 16. Subxiphoid cardiac view with no pericardial effusion and labeled chambers. Please note that the liver is in the near field. Image courtesy Drs. Douglas Franzen and Michael Vbralik from University of Washington.
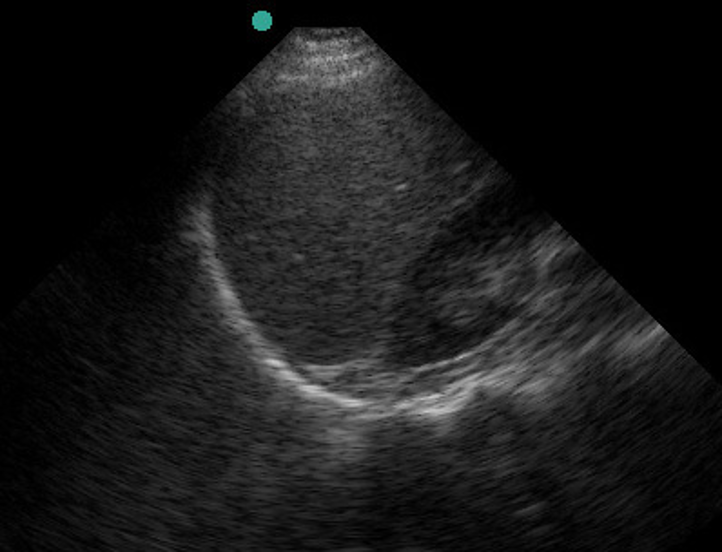

Figure 17. RUQ coronal view with a normal liver/kidney interface (top) and with fluid in Morrison’s pouch (bottom). Image courtesy Drs. Douglas Franzen and Michael Vbralik from University of Washington.
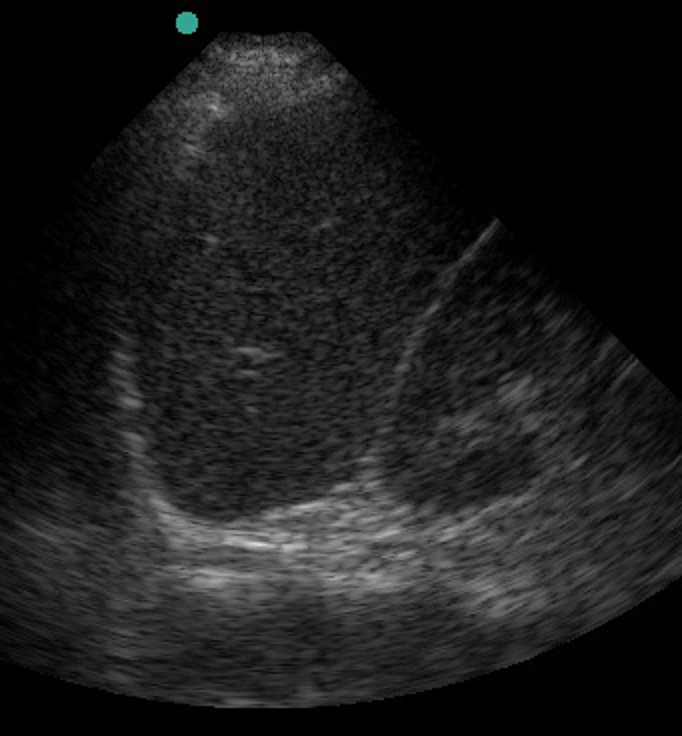
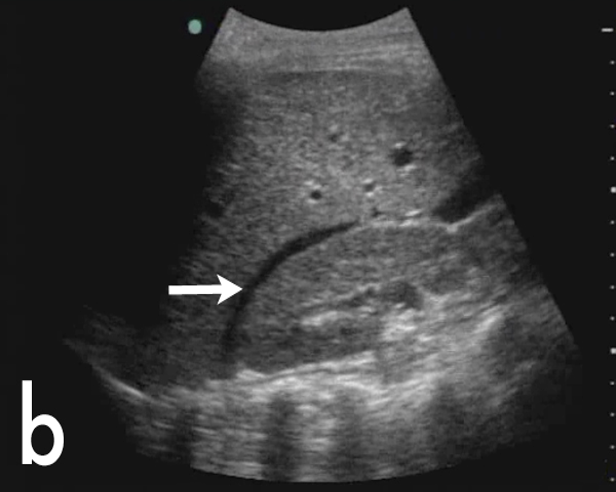
Figure 18 LUQ. coronal view with a) normal spleen/kidney interface. Image courtesy Drs. Douglas Franzen and Michael Vbralik from University of Washington.
 a a |  b b |
c
Figure 19. Normal female pelvis showing relationship of uterus and bladder in a) sagittal long-axis plane and b) transverse axial plane c) large amount of free fluid in rectouterine space (Images courtesy of Matthew Lohse, MD, Baylor Scott & White-Temple)
Notably, in the last 5-10 years the Extended FAST exam has become widely adopted at trauma centers, which adds assessment for pneumothorax and pleural fluid to the peritoneal and pericardial space evaluations. This EFAST exam hastens the diagnosis of important entities such as tension pneumothorax and massive hemothorax which may cause hemodynamic instability in the traumatically injured patient. Anterior lung fields are examined for “lung sliding,” which is the movement of the visceral lung pleura against the parietal chest wall pleura (Video 1). If present in the most anti-dependent region of the supine patient’s chest (Figure 20), lung sliding rules out pneumothorax with greater sensitivity than AP supine chest x-ray (REF. 6). Ultrasound can also detect as little as 20cc of pleural fluid, as seen in Figure 21.
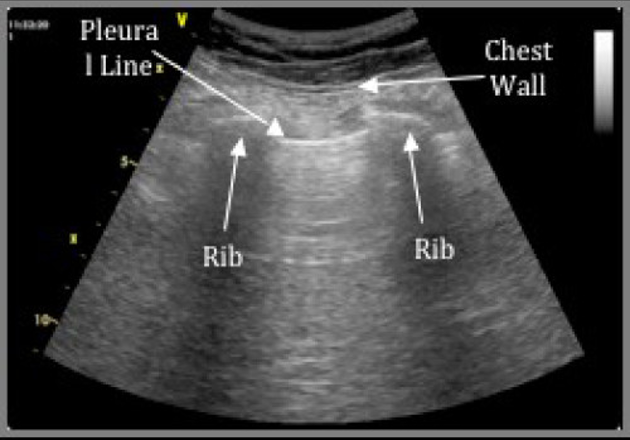 |  |
Figure 20. Anterior thorax sagittal lung view positioned at nipple line for maximum sensitivity for detecting pneumothorax. The white pleural line is examined for lung sliding motion (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple)
{left is normal, right with pneumothorax}
Video 1. Lung sliding present on the left and absent on the right. (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple)

Figure 21. Shows a collection of blood above (to the left on the figure denoted by asterisks) the diaphragm on this Hepatorenal view ultrasound (courtesy of Creagh Boulger MD, The Ohio State University Wexner Medical Center).
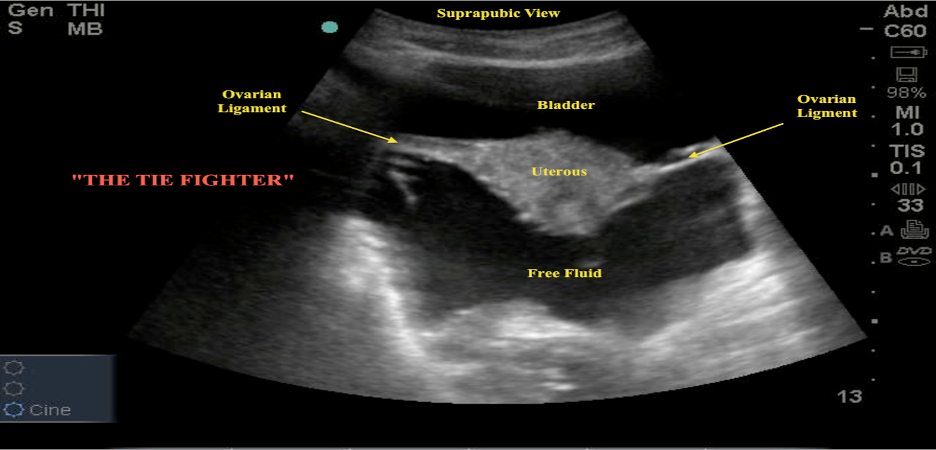
Intrauterine pregnancy
Pregnant patients often present to the Emergency Department in the first trimester with a variety of complaints, including vaginal bleeding, abdominal pain, and nausea/vomiting. The possibility of ectopic pregnancy in these patients is a major concern and should be ruled out. Emergency ultrasound can be used in the setting of pregnancy to evaluate for the presence or absence of intrauterine pregnancy. The images of Figure 22 demonstrate a gestational sac, the earliest finding of pregnancy by ultrasound, and the adjacent image shows a yolk sac, which is the minimum finding needed to confirm intrauterine pregnancy (IUP). A finding of intrauterine pregnancy (Video 2) in most patients effectively rules out ectopic (Video 3) or heterotopic pregnancy, which is the simultaneous presence of IUP and ectopic pregnancy (REF. 2 & 3).
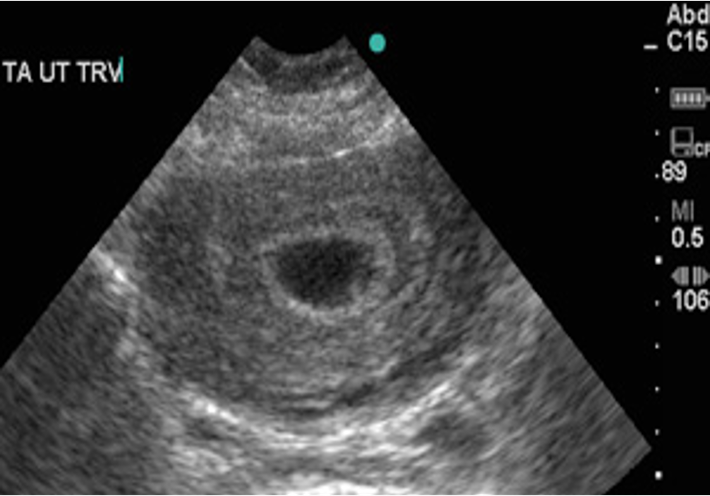 | 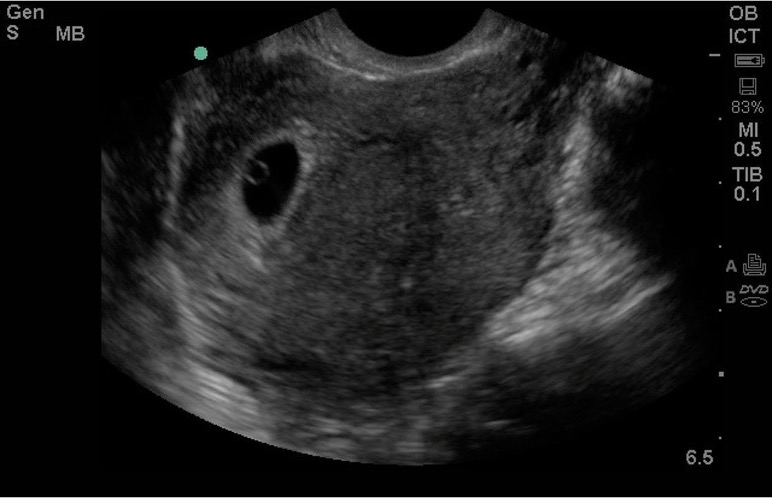 |
Figure 22. Gestational sac seen on left, yolk sac present as ring within the gestational sac on the right image (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Video 2. Transabdominal scan of uterus containing an intrauterine pregnancy with yolk sac inside gestational sac (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Video 3. Transabdominal scan showing live adnexal ectopic pregnancy with fetal heart rate flicker evident (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Abdominal Aortic Aneurysm
Abdominal aortic aneurysm (AAA) is a relatively common finding in patients over 50 years of age, especially with smoking history, and can be evaluated using emergency ultrasound. Dilation of the abdominal aorta greater than 3 cm indicates AAA and patients with dilation greater than 5 cm (Figure 23) are at increased risk for spontaneous rupture of the aorta (REF. 9). In patients with symptoms concerning for ruptured AAA, clinician-performed ultrasound can speed diagnosis and treatment in this life-threatening condition.
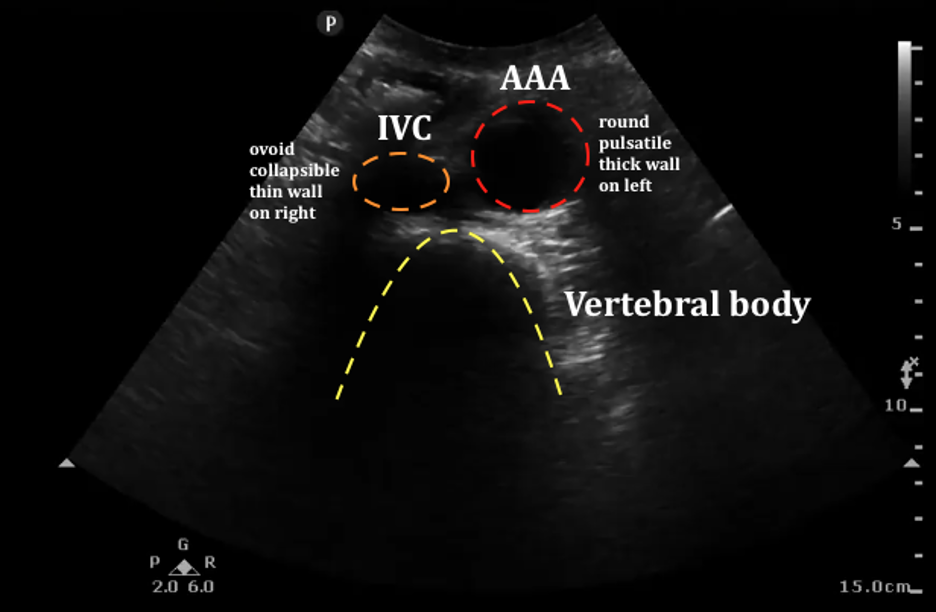
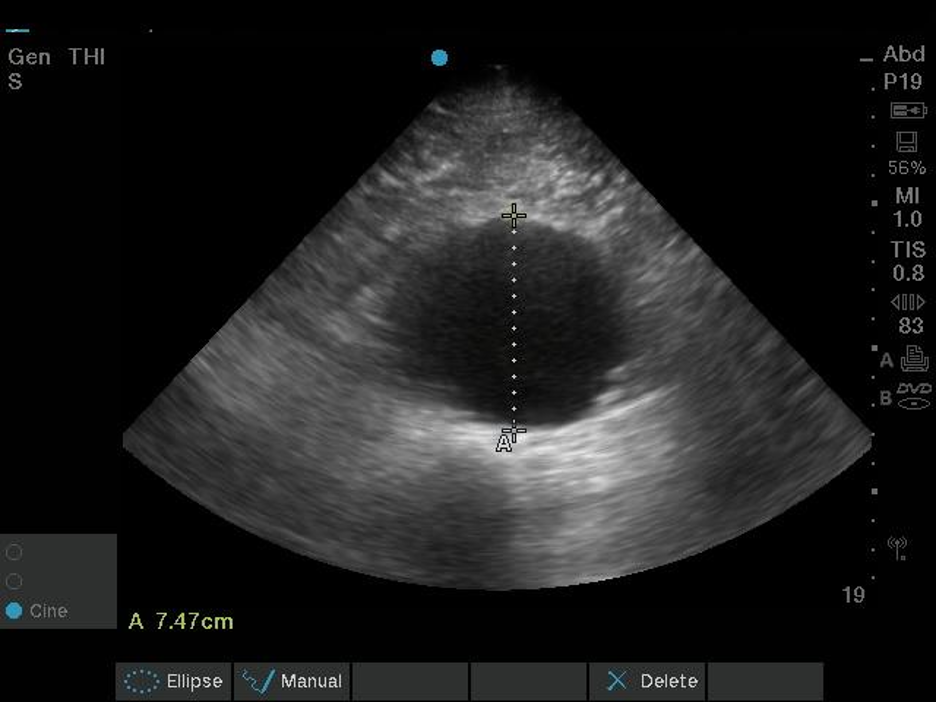
Figure 23. Upper image with normal abdominal aorta localized anterior to the spine (arrow), bottom image with large AAA. Upper image Courtesy of emDocs and is used under the Creative Commons Attribution 4.0 International License. The original image is located at: emDOCs.net – Emergency Medicine EducationUS Probe: Ultrasound for Abdominal Aortic Aneurysm - emDOCs.net - Emergency Medicine Education. The lower image is courtesy of Taming the SRU and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original image is located at: US - Abdominal Aortic Aneurysm - Ultrasound Case of the Month — Taming the SRU.
Aortic dissection can also be assessed with emergency ultrasound and the finding of an intimal flap (Video 4) is pathognomonic for this important pathologic process.
Video 4. Longitudinal view of abdominal aorta anterior to vertebral column demonstrating a bright hyperechoic intimal flap (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple)
Cardiac/Hemodynamic Assessment
Clinician-performed transthoracic cardiac ultrasound is indicated in patients with significant hemodynamic compromise. It is used to assess overall cardiac function and left ventricular contractility (Video 5) and to rapidly identify potentially reversible conditions such as pericardial effusion and tamponade. Other indications for cardiac ultrasound include assessment for signs of right heart strain (often from pulmonary embolism), volume status and thoracic aortic dissections.
Video 5. Parasternal long axis clip with severely reduced left ventricular ejection fraction (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
The standard cardiac views include the subxiphoid/subcostal, parasternal long axis, parasternal short axis and apical four-chamber.
Biliary
Biliary pathology including cholelithiasis causing biliary colic and cholecystitis is a common finding in patients presenting to the emergency department with abdominal pain. Emergency ultrasound can hasten diagnosis and surgical consultation. The primary sonographic abnormalities noted in patients with biliary disease include the presence of gallstones, which are round, hyperechoic objects with posterior acoustic shadowing. Ultrasound criteria for cholecystitis include:
Gallbladder wall thickening >3mm
Pericholecystic fluid
Sonographic Murphy’s sign (Figure 24) (REF. 10)

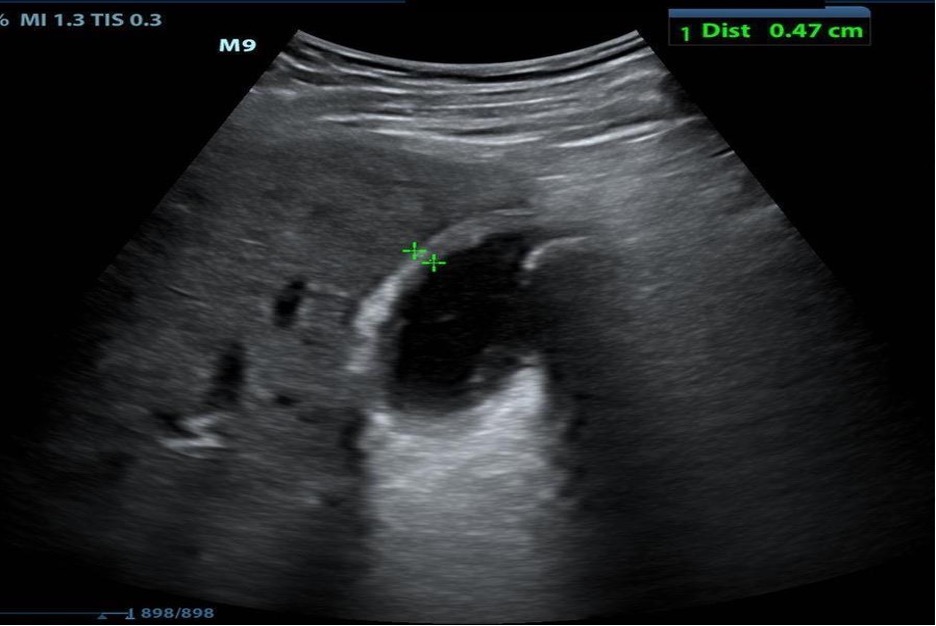
Figure 24. Top image showing gallstones with characteristic shadowing artifact; bottom showing wall-thickening and pericholecystic fluid in cholecystitis (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Urinary Tract
Flank pain or renal colic due to the presence of ureterolithiasis is a common presenting complaint in the emergency department. The presence of hydronephrosis (Figure 25) identified with ultrasound in patients with classic symptoms of renal colic, such as flank pain and hematuria, is highly suggestive of ureterolithiasis as the cause of the patient’s symptoms.


Figure 25. Moderate hydronephrosis of the right kidney (top image) upstream from the ureterovesicular junction stone marked with calipers seen near the bladder (bottom) (Images courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Ureteral jets (Video 6) can also be assessed with power Doppler and may provide additional information as to the degree of ureteral obstruction.
Video 6 Transverse bladder view illustrating use of power Doppler to visualize a right ureteral jet of urine (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a common cause of lower extremity pain and swelling which can be readily diagnosed at the bedside with ultrasound (REF. 11). The transducer is used to compress the deep veins of interest to assess for patency and the presence of thrombus. A non-compressible venous blood vessel indicates the presence of thrombus (Video 7).
Video 7. Right common femoral vein doesn’t fully compress at the level of the saphenous junction, and an echogenic thrombus is visualized (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Soft Tissue/Musculoskeletal
Ultrasound has great utility for evaluating soft tissue for the presence of abscess or cellulitis (Figure 26). Other musculoskeletal applications include evaluation of ligamentous and tendinous structures for common injuries, such as Achilles tendon rupture. Fractures can also be easily visualized with ultrasound, and ultrasound can be used to confirm glenohumeral shoulder dislocation/reduction status more expediently than x-ray (REF. 12).

Figure 26. Large anechoic abscess cavity in abdominal wall panniculus (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Thoracic/Airway
Common emergency department thoracic pathologies detectable with ultrasound include pneumothorax, pleural effusion, pulmonary edema and pneumonia. In Figure 27, the right lung can be seen surrounded by a large right sided pleural effusion. Emerging airway applications include confirmation of tracheal vs. esophageal position of an endotracheal tube. In anticipated difficult airway scenarios where neck anatomy isn’t easily palpable, such as post-radiation, post-surgical, or morbidly obese patients, ultrasound can be used to identify the cricothyroid membrane as in Figure 28 below (REF. 13).

Figure 27. Large right pleural effusion seen from coronal midaxillary plane (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
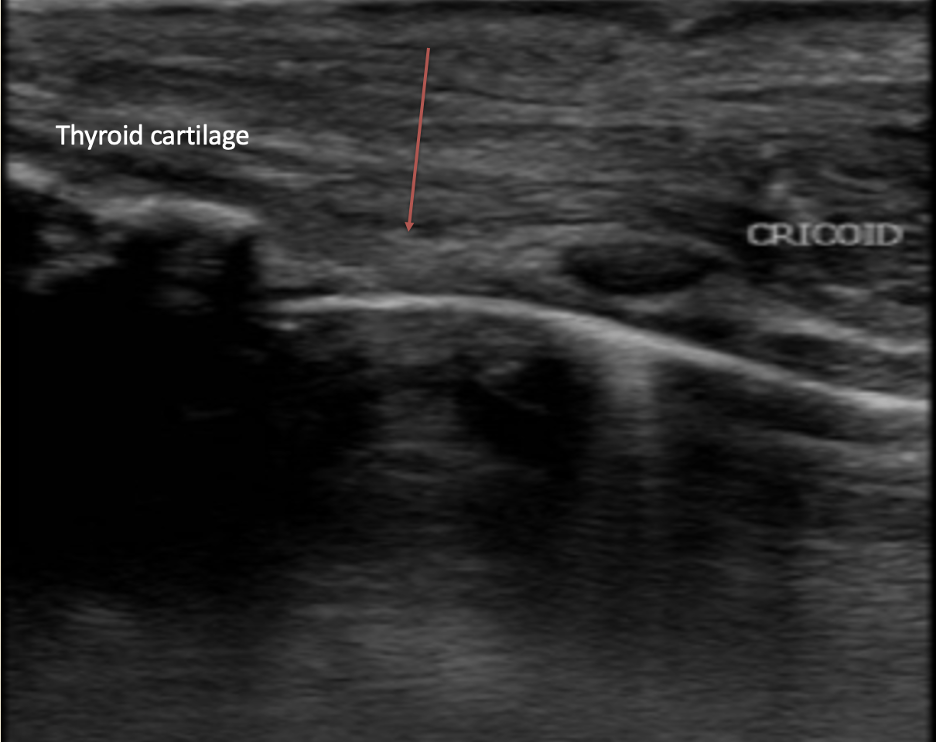
Figure 28. Sagittal section of trachea, a white hyperechoic line representing the air mucosal interface, with red arrow indicating cricothyroid membrane (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Ocular
Ocular ultrasound (Figure 29) can be used to evaluate for ocular pathologies such as foreign body, lens dislocation, vitreous hemorrhage and retinal detachment (REF. 5). Additionally, ultrasound can be used to evaluate patients with potentially increased intracranial pressure by evaluating the optic nerve sheath diameter.

Figure 29. Transverse image of eye demonstrating anatomy (Image courtesy of Matthew Lohse, MD. Baylor Scott & White-Temple).
Procedural Guidance
Many medical procedures performed in the Emergency Department can be done with the assistance of ultrasound. Examples include:
Central venous catheter placement
Peripheral venous catheter placement
Peritonsillar and cutaneous abscess drainage
Trans-venous cardiac pacer lead placement
Paracentesis
Thoracentesis
Arthrocentesis.
Other emerging and more advanced emergency ultrasound applications discussed in the ACEP 2016 guidelines include advanced echocardiography, transesophageal echocardiography, bowel evaluation (including intussusception, appendicitis, pyloric stenosis, diverticulitis and small bowel obstruction), adnexal pathology, testicular ultrasound, transcranial Doppler, and contrasted studies (REF. 5). Clearly, the use of ultrasound is continuing to rapidly evolve and expand in the field of emergency medicine, and many other medical specialties are adopting clinician-performed bedside ultrasound into regular clinical practice in an effort to improve patient care.
Pearls and Pitfalls
Position patient prior to exam to maximize sonographer and patient comfort.
Knowledge of surface anatomy and underlying structures aids in initial placement of transducer for rapid identification of anatomy of interest.
Obtain a solid understanding and ability to obtain the basic views for each study before moving on to more difficult applications.
Inadequate use of gel or incomplete contact of transducer footprint with patient skin can limit the image quality of relevant anatomy.
A negative EFAST exam does not rule out traumatic intra-abdominal injury, it just helps to rule out hemodynamically consequential sources of hemorrhage during the primary survey. If traumatic mechanism is significant and patient has significant abdominal pain or tenderness, a CT is still indicated.
Be aware of anatomical variants (e.g. horseshoe kidney, duplication of the popliteal veins) which may confuse the novice sonographer
Remember that emergency ultrasound diagnoses of pathology do not usually provide the final word in the workup, but they often provide the first!
Case Study Resolution
You return to the patient’s bedside with your ultrasound in tow, noting repeat BP is now 95/70, HR 110, and perform an abdominal aorta study, noting there is a 6.5 cm infrarenal AAA with some anechoic fluid anterior to it in the retroperitoneum. While obtaining a rapid istat creatinine and hematocrit and wheeling the patient to CT for an angiogram to further elucidate your findings, you order the patient type and crossmatched for 6 units RBCs and page vascular surgery. They arrive 5 minutes later and rush the patient to the OR for endovascular repair. You get a page 15 minutes after the patient has left the ED from the radiologist with the critical finding on CT. You nonchalantly thank them for the call, letting them know the patient is already in the OR, and then go to see your next patient.
References
Edelman SK. Understanding Ultrasound Physics, Third Ed. ESP Ultrasound. 2004.
Noble VE, Nelson BA, Sutingco AN. Manual of Emergency and Critical Care Ultrasound. Cambridge University Press. 2007.
Ma O, Mateer JR, Reardon RF, Joing SA. eds. Ma and Mateer's Emergency Ultrasound, 3e. McGraw Hill. 2014.
Shah S, Price D. eds. Manual of Ultrasound for Resource Limited Settings. Partners in Health. 2011.
Ultrasound Guidelines: Emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med. 2017 May;69(5):e27-e54.
Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010 Jan;17(1):11-7.
Richards SR, Stempel LE, Carlton BD: Heterotopic pregnancy: Reappraisal of incidence. Am J Obst Gynecol 142:928, 1982.
Bello GV, Schonolz D, Moshirpur J, et al: Combined pregnancy: The Mount Sinai experience. Obstet Gynecol Surv 41:603, 1986.
Brewster, D.C., Cronenwett, J.L., Hallett, J.W. Jr, Johnston, K.W., Krupski, W.C., Matsumura, J.S. Guidelines for the treatment of abdominal aortic aneurysms (Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery) . J Vasc Surg. 2003;37:1106–1117.
Pinto A, Reginelli A, Cagini L, et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J. 2013;5:S11.
Bernardi E, Camporese G, Buller HR, et al. Serial 2-point ultrasonography plus d-dimer vs whole-leg color-coded Doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis: a randomized controlled trial. JAMA. 2008;300(14):1653–9.
Secko MA, Reardon L, Gottlieb M, Morley EJ, Lohse MR, Thode HC Jr, Singer AJ. Musculoskeletal Ultrasonography to Diagnose Dislocated Shoulders: A Prospective Cohort. Ann Emerg Med. 2020 Aug;76(2):119-128
Yildiz F, Goksu E, Senfer A et al. Comparison of ultrasonography and surface landmarks in detecting the localization for cricothyroidotomy. Am J EmergMed. 2016;34: 254-256.
