Elder Mistreatment
Authors: Surriya Ahmad MD, Tony Rosen MD
Edited By: Angel Li MD; Shan Liu MD, SD
Updated: 9/24/2021
Case Study
An 80-year-old man who lives alone but has assistance of a home health aide for 12 hours per day is brought to the emergency department (ED) by his daughter, who went to visit and found him with severe bruising. On examination, he had multiple bruises at varying stages of healing on the chest and bilateral arms, as well as a linear patterned injury across his left anterior chest. What should you do next?
Objectives
By the end of this module, the student will be able to:
- Identify potential cases of elder mistreatment in the ED by recognizing:
- Concerns about older adult/caregiver interactions that may be suspicious for elder abuse or neglect
- Concerns about the patient’s medical history and home environment that are suspicious for elder abuse
- Injury patterns and other physical signs suspicious for elder abuse
- Risk factors for elder abuse victimization and perpetration
- Intervene appropriately once elder mistreatment is suspected or confirmed, including reporting and ensuring a safe disposition plan
Introduction
Elder mistreatment, which includes physical abuse, sexual abuse, neglect, and emotional/psychological abuse, is common and may have serious medical and social consequences. As many as 10% of older adults living in the community, and more than 20% of nursing home residents experience some form of abuse, neglect, or exploitation each year. Elder mistreatment is under-recognized by emergency clinicians and under-reported to the authorities.
Initial Actions
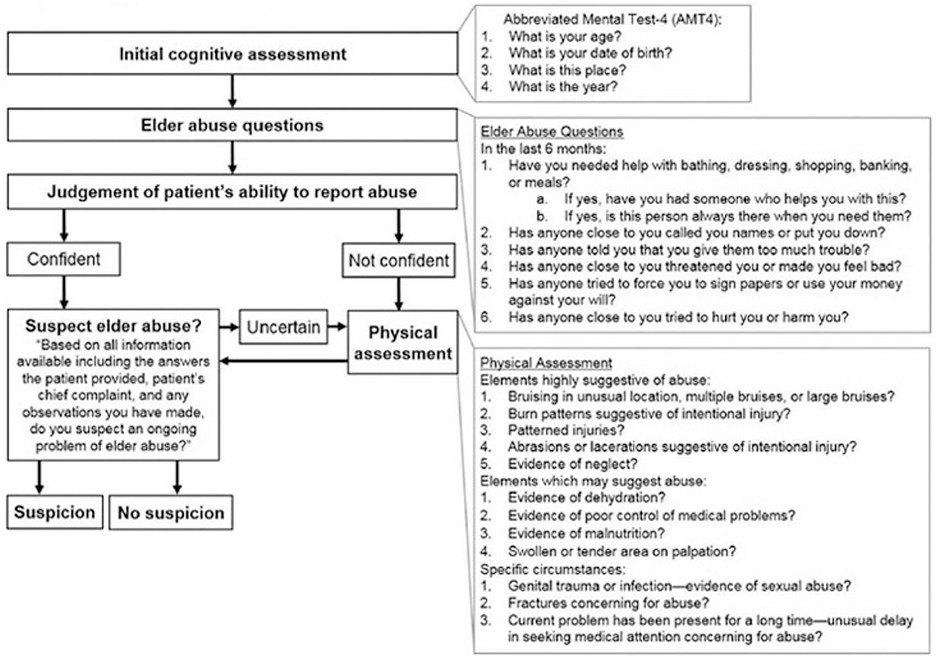
The ED provider should always observe patient/caregiver interactions if a caregiver is present at the bedside, watching for anything suggestive of potential mistreatment (see Table 1). A complete and accurate medical history is also critical to identify elder mistreatment. Indicators of mistreatment in the medical history are shown in Table 2. When feasible, the ED provider should take the medical history from the patient alone without caregivers or family present and should assure the patient of privacy and confidentiality (see Table 2). Attempting to speak to the patient is particularly important even if it appears as though they will not be able to provide a history due to dementia or other cognitive impairment, as subtle clues may be picked up. A recent study found that a vast majority of patients with mild cognitive impairment were able to accurately report elder abuse. (Ref. 2) (see Table 3) ED providers should also attempt whenever possible to separately interview the caregiver or suspected abuser, as this could potentially reveal discrepancies from the patient’s history which may illuminate abuse or neglect.
Table 1: Observations from older adult/caregiver interaction that should raise concern for elder mistreatment
Data from reference 1 |
Table 2: Indicators from the medical history of possible elder mistreatment
Data from reference 1 |
Table 3: Potential risk factors for elder mistreatments
For becoming a victim:
For becoming a perpetrator:
Data from references 1, 10-13 |
Performing a comprehensive physical exam is essential to adequately evaluate for elder mistreatment (see Table 4). ED providers concerned with mistreatment should document their findings in detail with complete descriptions of all physical findings, including even minor injuries, and should consider photographing findings or using a body diagram/traumagram.
Table 4: Physical signs suspicious for potential elder abuse or neglect
Physical abuse
Sexual abuse
Neglect
Data from references 1, 14-19 |
Targeted Screening: ED Senior AID
Elder mistreatment is common, missing it is catastrophic, and the ED visit represents a rare opportunity for intervention before it is too late. Most common screening consists of a single question about home safety, and it is generally accepted that this single question is inadequate and often represents a missed opportunity for identification. ED Senior AID is a multicenter validated screening tool for elder abuse with 94% sensitivity and 84% specificity.
Laboratory Testing
Although no laboratory blood or urine test is definitively diagnostic for elder mistreatment, certain findings may raise or increase suspicion, including anemia, dehydration, malnutrition, hypothermia/hyperthermia, and rhabdomyolysis. (Ref. 20) Also, ED providers should consider checking prescription medication and illicit drug levels. Low or undetectable levels may indicate withholding by a caregiver, elevated drug levels may indicate overdose, and the presence of toxins of drugs that have not been prescribed may indicate poisoning. (Ref. 20)
Imaging
Limited radiology literature exists describing potential imaging correlates of elder mistreatment. (Ref. 21-23) Findings suggestive of mistreatment may include co-occurring old and new fractures, high injury fractures with low energy mechanism, distal ulnar diaphyseal fractures, and small bowel hematomas. (Ref. 21-23) The ED provider should communicate any suspicion for elder mistreatment to the radiologist and ask them to focus on whether the imaging findings are consistent with the purported mechanism. Providers may also consider additional screening imaging tests, including maxillofacial computed tomography scan and chest X ray, to evaluate for acute and chronic fractures -- analogous to the skeletal survey routinely performed in potential victims of child abuse.
Treatment
When elder mistreatment is suspected or confirmed, an ED provider should 1 treat acute medical, traumatic, and psychological issues; 2 ensure patient safety; and 3 report to the authorities. Address ABCs (Airway, Breathing, Circulation) first as well as the patient’s injuries. Consider unique challenges for a geriatric patient in the ED, and maintain comfort as much as possible, taking into account psychosocial and psychological issues and providing appropriate resources. ED clinicians should report potential cases of elder mistreatment to the appropriate authorities, and ensure the patient has a safe disposition.
A team-based multidisciplinary approach in the ED can be fundamental in optimizing chances for detection of elder mistreatment in the ED and managing next steps post detection. From EMS to the triage team, nursing interactions at bedside, techs, radiologists, clerks, transport, and social work, an ED visit provides multiple chances at detection, and a collaborative approach is absolutely vital to maximizing each chance.
Pearls and Pitfalls
- Elder mistreatment, which includes physical abuse, sexual abuse, neglect, emotional/psychological abuse, abandonment, financial/material exploitation, and self-neglect, is common and may have serious medical and social consequences, but is often under-recognized by emergency clinicians and under-reported to the authorities.
- Emergency clinicians must maintain a high index of suspicion for elder mistreatment even when signs or symptoms suggest otherwise. Particular care should be taken in medical history, physical examination, medical/laboratory markers, and radiological studies.
- Patients and caretakers should be interviewed separately.
- Emergency clinicians should document completely and accurately the history and all physical findings in cases of suspected elder mistreatment, as this documentation may be critical to ensure justice for the victim.
- ED Senior AID is a validated screening tool for use in the ED with high sensitivity and specificity.
- Using a team-based approach including social workers, other ED-based professionals, and Emergency Medical Services can play a critical role in improving elder mistreatment detection.
- ED management of elder mistreatment should include: treating acute medical and psychological issues, ensuring patient safety, and proper reporting to the authorities. Trauma-informed care should be provided.
- Elderly patients who are in immediate danger should be hospitalized, or a care plan should be implemented that prevents them from having any contact with the suspected abuser(s). If an older adult with decision-making capacity refuses interventions and desires to return to an abusive situation, his or her wishes must be respected, and appropriate resources must be provided prior to disposition.
Case Study Resolution
The patient’s ABCs are intact, and after the complete physical exam, the caregiver and patient are interviewed separately. The patient is asked questions in a non-threatening manner. The central and bilateral locations of the contusions and linear pattern of the bruise on the left side of the chest are highly suggestive of physical abuse. Suspicion for elder mistreatment is high and a report is filed with APS.
References
- Rosen T, Stern ME, Elman A, Mulcare MR. Identifying and initiating intervention for elder abuse and neglect in the Emergency Department. Clin Geriatr Med 2018;34:435-451.
- Richmond, et al. Ability of Older Adults to Report Elder Abuse: An Emergency Department–Based Cross-Sectional Study. J Am Geriatr Soc 68:170-175, 2020.
- Wiglesworth A, Mosqueda L. People With Dementia as Witnesses to Emotional Events. Washington, DC: National Institute of Justice; 2011.
- Alsawy et al. ‘It’s nice to think somebody’s listening to me instead of saying “oh shut up”’. People with dementia reflect on what makes communication good and meaningful. Journal of Psychiatric and Mental Health Nursing. 26 August 2019. https://doi.org/10.1111/jpm.12559
- Portacolone et al. Expectations and Concerns of Older Adults With Cognitive Impairment About Their Relationship With Medical Providers: A Call for Therapeutic Alliances. Qual Health Res. 2020 Aug; 30(10): 1584–1595.
- Brod M, Stewart AL, Sands L, P W. Conceptualization and measurement of quality of life in dementia: the dementia quality of life instrument (DQoL). Gerontologist. 1999;39:25-36.
- Dong X, Simon M, Rajan K, Evans DA. Association of cognitive function and risk for elder abuse in a community-dwelling population. Dement Geriatr Cogn Disord 2011;32:209-215.
- Pillemer K, Burnes D, Riffin C, Elder abuse LMS. global situation, risk fac- tors, and prevention strategies. Gerontologist. 2016;56:S194-S205.
- Beach SR, Carpenter CR, Rosen T, Sharps P, Gelles R. Screening and detec- tion of elder abuse: research opportunities and lessons learned from emer- gency geriatric care, intimate partner violence, and child abuse. J Elder Abuse Negl. 2016;28:185-216.
- Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health 2010; 100:292–7.
- Amstadter AB, Zajac K, Strachan M, et al. Prevalence and correlates of elder mistreatment in South Carolina: the South Carolina elder mistreatment study. J Interpers Violence 2011;26:2947–72.
- Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci 2008;63:S248–54.
- Pillemer K, Burnes D, Riffin C, et al. Elder abuse: global situation, risk factors, and prevention strategies. Gerontologist 2016;56(Suppl 2):S194–205.
- Collins KA. Elder maltreatment: a review. Arch Pathol Lab Med 2006;130:1290–62.
- Speck PM, Hartig MT, Likes W, et al. Case series of sexual assault in older persons. Clin Geriatri Med 2014;30:779–806.
- Gibbs LM. Understanding the medical markers of elder abuse and neglect: phys- ical examination findings. Clin Geriatr Med 2014;30:687–712.
- Palmer M, Brodell RT, Mostow EN. Elder abuse: dermatologic clues and critical solutions. J Am Acad Dermatol 2013;68:e37–42.
- Chang AL, Wong JW, Endo JO, et al. Geriatric dermatology: part II. Risk factors and cutaneous signs of elder mistreatment for the dermatologist. J Am Acad Dermatol 2013;68:533.e1-10 [quiz: 43–4].
- Rosen T, LoFaso VM, Bloemen EM, Clark S, McCarthy TJ, Reisig C, Gogia K, Elman A, Markarian A, Flomenbaum NE, Sharma R, Lachs MS. Identifying Injury Patterns Associated With Physical Elder Abuse: Analysis of Legally Adjudicated Cases. Ann Emerg Med. 2020 Sep;76(3):266-276.
- LoFaso VM, Rosen T. Medical and laboratory indicators of elder abuse and neglect. Clin Geriatr Med 2014;30:713–28.
- Murphy K, Waa S, Jaffer H, et al. A literature review of findings in physical elder abuse. Can Assoc Radiol J 2013;64:10–4.
- Rosen T, Bloemen EM, Harpe J, et al. Radiologists’ training, experience, and at- titudes about elder abuse detection. AJR Am J Roentgenol 2016;207:1210–4.
- Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J 2017;68:16–20.
- Rosen T, Platts-Mills TF, Fulmer T. Screening for elder mistreatment in emergency departments: current progress and recommendations for next steps. J Elder Abuse Negl. 2020 Jun;32(3):295-315
- Olsen, et al. Screening for Elder Abuse in the Emergency Department, ppt. AGS.
- Rosen et al. Identifying Elder Abuse in the Emergency Department: Toward a Multidisciplinary Team-Based Approach. Ann Emerg Med 2016 Sep;68(3):378-82.
- Bloemen et al. Elder Mistreatment & Abuse: Assessment and Teamwork, ptt. AGS
- Chapter 181: Geriatric Abuse and Neglect. Rosen’s Textbook of Emergency Medicine v11. Rosen