Hyperkalemia
Author: Tracy MacIntosh MD, University of Central Florida/Osceola Regional Medical Center.
Editor: George Willis MD, University of Maryland School of Medicine
Last Updated: 2019
Case Study
68 year-old gentleman with a history of diabetes, hypertension, coronary artery disease and chronic kidney disease presents to the Emergency Department (ED) with generalized weakness, fatigue and lightheadedness following a weeklong illness during which his wife reports he has complained of nausea and had a poor appetite. The patient states he had a CT scan performed at another hospital and was told that there was “nothing wrong.”
Objectives
- Describe the classic presentation of a patient with hyperkalemia
- Describe risk factors for developing hyperkalemia
- Identify electrocardiographic manifestations of hyperkalemia
- List the principles of managing a patient with hyperkalemia
Introduction
Hyperkalemia is a potentially life-threatening electrolyte abnormality seen frequently in the ED. The most common condition leading to hyperkalemia is missed dialysis in a patient with end stage renal disease (ESRD), but many other conditions can predispose an individual to hyperkalemia.
The etiologies of hyperkalemia can grouped in three categories:
- Decreased renal clearance including chronic kidney disease (CKD) or acute kidney injury (AKI). Potassium homeostasis is well maintained through renal mechanisms. Any process that impedes the excretion of through the renal tubules can cause increased serum concentrations.
- Increased release from intracellular space (e.g. hemolysis, rhabdomyolysis, burns or crush injury). The release of intracellular potassium is often worsened by a coinciding decrease in the renal excretion.
- Altered transfer to the intracellular space (e.g. acidosis, insulin deficiency, succinylcholine). These causes are typically transient and can be affected rapidly by interventions such as correction of acidosis and administration of fluids.
Hyperkalemia changes the electrochemical gradient of cells, making muscle weakness and cardiac dysrhythmias potentially fatal outcomes to undiagnosed abnormalities. Rapid identification and appropriate treatment are paramount to properly treating this condition.
Initial Actions and Primary Survey
The primary survey should focus on assessing airway, breathing and circulation (ABC). Since many patients with severe hyperkalemia will have renal dysfunction, some may be fluid overloaded and may present with pulmonary edema and respiratory distress.
Traditionally, the electrocardiogram (ECG) has been used as a surrogate marker for clinically significant hyperkalemia. Patients suspected of having hyperkalemia (e.g. chronic renal failure, severe diabetic ketoacidosis, etc.) should be placed on a cardiac monitor and a 12-lead electrocardiogram should be performed immediately. Concurrently, intravenous access should be obtained and a blood sample should be sent to the laboratory for a basic metabolic profile.
Presentation
The classic presentation of hyperkalemia is typically underwhelming. No signs or symptoms are pathognomonic for this condition, although patients may rarely present with weakness or paresthesias.
It is not uncommon for a patient with mild to moderate hyperkalemia to be identified by an unexpected laboratory abnormality.
Only in severe hyperkalemia do symptoms develop, with cardiovascular, neuromuscular, and gastrointestinal manifestations. One of the most common complaints in patients with severe hyperkalemia is weakness, however this complaint is neither sensitive nor specific for hyperkalemia and will also be seen with numerous other conditions.
With severe hyperkalemia, the most significant effect is on the cardiovascular system with dysrhythmias including 2nd or 3rd degree heart block, wide complex tachycardias, and progression to ventricular fibrillation and asystole. The clinician should have a high index of suspicion for hyperkalemia in patients with chronic renal failure and other predisposing conditions, particularly in the setting of hypotension or shock.
With moderate to severe hyperkalemia, patients may also develop gastrointestinal effects such as nausea, vomiting, and diarrhea or more commonly, neuromuscular effects, including muscle cramps, generalized weakness, paresthesias, tetany, and focal or global paralysis.
The physical examination of these patients tends to be unremarkable; however, look for extrasystoles, pauses or bradycardia on cardiac exam, decreased deep tendon reflexes or overall decreased strength on neurologic exam. Also evaluate specifically for evidence of chronic renal failure such as evidence of fluid overload and dialysis access sites.
Diagnostic Testing
Hyperkalemia is diagnosed by serum sampling, and is defined as a measured serum potassium greater than 5.5 mEq/L. A common cause of hyperkalemia is laboratory error resulting from a hemolyzed specimen, and this should be suspected in a patient with normal kidney function in the absence of ECG changes. Other less common etiologies of elevated potassium levels in the serum is pseudohyperkalemia resulting from thrombocytosis, leukocytosis or erythrocytosis. Hyperkalemia in the chronic renal failure patient is the most common cause of true hyperkalemia in the emergency department.
The ECG is a rapid, non-invasive and highly sensitive screening tool that can be used to evaluate patients suspected of having hyperkalemia.ECG abnormalities reflect the rate of rise of potassium and determine whether a given potassium level will cause cardiac arrest. Tall, peaked T waves are typically the earliest manifestations of hyperkalemia and occur before changes to the QRS complex. In the absence of any other ECG findings, peaked T waves are rarely associated with life-threatening arrhythmias.
QRS complex changes (uniform widening) are often evident with increasingly worsening hyperkalemia. Loss of P waves then follows, ultimately leading to the formation of sine-waves - the fusion of wide QRS complexes with ST-T segments.
Additionally, severe hyperkalemia can manifest with sinus bradycardia or arrest, AV blocks and loss of pacemaker capture. Impaired conduction in the His-Purkinje system from hyperkalemia and can also occur, causing fascicular and bundle branch blocks.
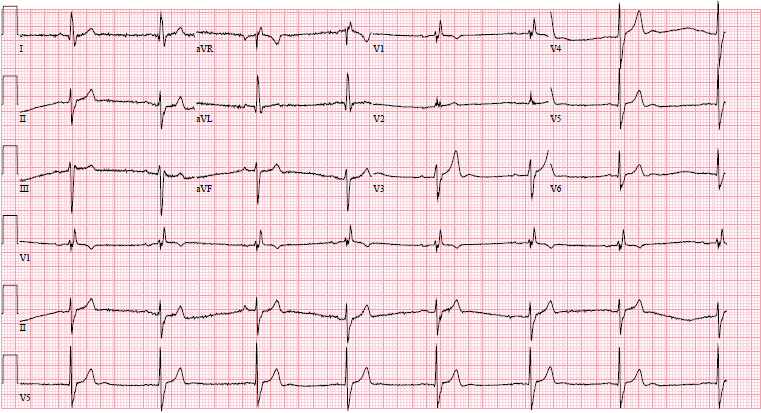
Figure 1.
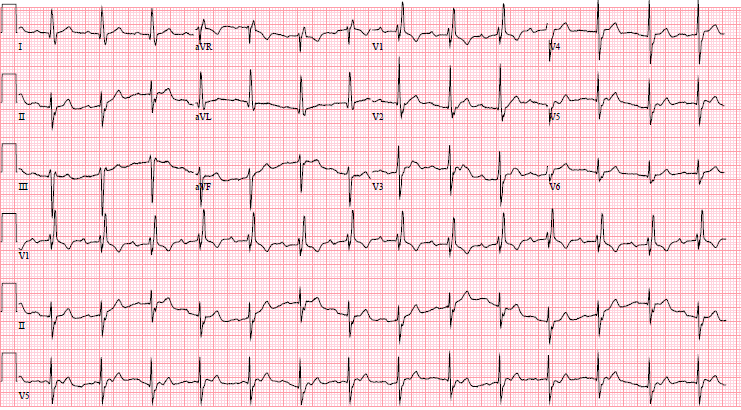
Figure 2
Serial ECG of patient with K+ of 6.7, hypotensive, demonstrating peaked T waves, sinus bradycardia, before (Fig.1) and after treatment (Fig.2). Used with permission from Joshua Tsau, MD.
Treatment
The urgency of treatment will depend primarily on whether ECG manifestations of hyperkalemia are present. When progressive ECG manifestations of hyperkalemia or hemodynamic instability are present, treatment is initiated first to stabilize the cardiac myocardium. Next, treatment is directed at shifting potassium from the extracellular to the intracellular space (potassium redistribution). Finally, treatment to rid the body of potassium is often necessary.
The mnemonic C BIG Potassium go Down is helpful for remembering the critical elements of hyperkalemia management:
C - Calcium salts
B - Beta-agonists
I - Insulin
G - Glucose (give with insulin)
P - Patiromer (relatively new, may not be available in the ED)
D - Dialysis or Diuretics
1. Stabilize the Cardiac Membrane
Calcium gluconate or calcium chloride (1 ampule or 1g) IV over 2-5 minutes; the effect is immediate. This dose may be repeated after 5 minutes if no improvement. Onset within minutes, and lasts approximately 30-60 minutes. Calcium chloride has three times more elemental calcium than calcium gluconate. However, calcium chloride may cause tissue necrosis if extravasation occurs. Therefore, it should only be given through a central line or if the patient has severe hemodynamic compromise or cardiac arrest. Intravenous calcium salts should be used with caution in patients with hyperkalemia and digoxin toxicity. Consider hypertonic saline (10ml of 3%) in this situation.
Remember that these medications are temporizing measures and do not lower the potassium levels. Further treatment to lower the potassium level is still required.
If there are no cardiac effects or hemodynamic instability, reconfirm the K+ with serum sampling prior to treatment.
2. Intracellular Potassium Transfer
- Regular insulin 5-10 units IV, combined with Dextrose (D50 50 ml), especially if the serum glucose is less than 250 mg/dL. Onset 15 minutes, duration 4-6 hours. Be sure to repeat a fingerstick in 30 minutes to make sure hypoglycemia doesn’t occur.
- Albuterol 10mg-15mg nebulized. Onset 60-90 minutes, duration 2-3 hours. This medication does not work in approximately 40% of the population, and will be significantly less effective in patients on beta-blockers, so always use this in conjunction with insulin.
- Sodium bicarbonate IV- now widely regarded as ineffective in the acute management of elevated potassium in patients with chronic renal failure. It may have a role in patients who have a severe metabolic acidosis.
3. Decrease Total Body Potassium
- Kayexalate – binding resin that exchanges sodium for potassium in the colon, onset 1-2 hours, duration 4-12 hours. No longer routinely given as it may have negative safety for patients. May still be requested by admitting services.
- Furosemide 20-40mg IV, onset 15 minutes to 1 hour, duration approximately 4 hours. May enhance renal excretion of potassium in patients with preserved renal function without urinary tract obstruction.
- Hemodialysis – indicated if hemodynamically unstable or the patient doesn’t make urine and is dialysis-dependent.
- Patiromer - 8.4g PO daily. Not indicated for emergent management of hyperkalemia due to delayed onset of action. It binds potassium in the GI tract and increases fecal excretion. Indicated in patients with CKD 3 and 4 or patients taking potassium-sparing diuretics or renin-angiotensin-aldosterone system inhibitors. This medication is not widely available yet.
Pearls and Pitfalls
- Obtain an ECG on patients with chronic kidney disease who present with generalized fatigue and weakness to quickly screen for hyperkalemia.
- Patients with no reason for hyperkalemia found incidentally should have the potassium level repeated to make sure hemolysis is not present.
- Calcium salts only stabilize the cardiac membrane and do nothing to lower the potassium level and further treatment is required to lower the potassium level.
Case Study Resolution
The patient’s ECG shows a wide QRS complex and peaked T waves concerning for hyperkalemia. Appropriate treatment with calcium gluconate, insulin, and dextrose is initiated empirically. The laboratory values show a potassium of 7.1 mEq/L with a serum creatinine of 4.6 mg/dL. Nephrology is consulted for hemodialysis. The patient is admitted to the hospital and stabilized, and is ultimately discharged home with improved renal function.
References
- Depret, F., et al., Management of hyperkalemia in the acutely ill patient. Ann Intensive Care, 2019. 9(1): p. 32.
- Littmann, L. and M.A. Gibbs, Electrocardiographic manifestations of severe hyperkalemia. J Electrocardiol, 2018. 51(5): p. 814-817.
- Mount, David B. “Causes and Evlaitjoma of Hyperkalemia in Adults.” UpToDate, 8 June 2019, www.uptodate.com/contents/causes-and-evaluation-of-hyperkalemia-in-adults?search=hyperkalemia%2Bcauses&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H783293332.
