Cardiac Arrest
Adult Basic and Advanced Life Support
Author Credentials
Author: Julianna Jung, MD, Associate Professor of Emergency Medicine, Johns Hopkins University School of Medicine (2023 Version). Emily Hillman, MD, Assistant Professor of Emergency Medicine, University of Missouri-Kansas City (Original Version)
Editor: Navdeep Sekhon, MD, Associate Professor of Emergency Medicine, Baylor College of Medicine
Updated: 8/14/2023
Case Study
You are a medical student on your Emergency Medicine clerkship. A 49-year-old man presents to the ED with chest pain. Shortly after arrival, he becomes acutely unresponsive. You realize that he’s apneic and pulseless, so you hit the code button and start CPR. The rest of your team comes rushing in and everyone is talking at once. A tech is putting defibrillation pads on the patient, one of the residents is trying to ultrasound the patient’s heart, and another is setting up to intubate. A nurse comes up with an amp of epinephrine, but the patient doesn’t even have access yet, and your attending is trying to decide whether to activate a STEMI alert.
There’s so much happening at once, but what’s the most important thing to do? When it’s your turn to be in charge of a code response, how should you prioritize and make sense of the chaos?
Objectives
By the end of this module, the student will be able to:
- Describe an approach to the initial assessment and stabilization of patients with cardiac arrest
- Discuss the importance of adequate chest compressions and early defibrillation in the management of pulseless patients
- Identify arrest rhythms on electrocardiogram, including ventricular fibrillation, ventricular tachycardia, pulseless electrical activity, and asystole
- Compare and contrast the treatment algorithms for each of the above rhythms
- Formulate a differential diagnosis for potentially reversible causes of cardiac arrest
Introduction
More than 300,000 out-of-hospital adult cardiac arrests occur each year in the United States and approximately 10% survive the arrest.(Ref.1-4) Around 200,000 in-hospital adult cardiac arrests occur every year and approximately 25% survive to hospital discharge.(Ref.3-6). This figure has climbed steadily from less than 17% in 2000. (Ref.4) Pediatric survival rates for in-hospital arrest are significantly higher than adult rates, currently at approximately 40%.(Ref.4) There are notable racial and economic disparities in cardiac arrest incidence and outcomes, with patients who are black or from lower socioeconomic status more likely to experience cardiac arrest, and less likely to survive.(Ref.4) Basic life support (BLS) is critical to saving lives, and high-quality CPR and early defibrillation can improve survival rates.(Ref.6)
Initial Actions and Primary Survey
All patients who collapse or are found unresponsive should be presumed to be in cardiac arrest until proven otherwise.
Assessment is the first step when encountering such a patient, with the goal of rapidly confirming or refuting the diagnosis of cardiac arrest. Assessment must take less than 10 seconds; if the diagnosis is uncertain after 10 seconds, proceed as though the patient is indeed in cardiac arrest.(Ref.7)
Assessment for patients in cardiac arrest: C-A-B
C: Circulation is the FIRST priority! Check this by palpating the carotid pulse for no more than 10 seconds. If no pulse is detected, chest compressions must be initiated immediately! Compressions should be given at a rate of 100-120 per minute and a depth of 2-2.4 inches. They should be as continuous as possible, and every effort should be made to avoid interruptions in compressions.(Ref.7)
A/B: Airway and breathing are much less important than circulation in patients with suspected cardiac arrest. During the circulation assessment, look for signs of respiratory effort. However, in a pulseless patient, respiratory support should never be initiated before chest compressions are underway - supporting circulation is the priority. Once chest compressions are started, breaths can be delivered using a bag-valve-mask device, ideally attached to supplemental oxygen when available. Rescuers should coordinate compressions to breaths with a 30:2 ratio until such time as an advanced airway is established.(Ref.7)
Defibrillation:
Rescuers should request that a defibrillator be brought to the scene as soon as possible. In US hospitals, defibrillators are almost universally available. In places of mass gathering, automated external defibrillators (AEDs) are becoming increasingly common. These devices are designed for laypeople, as they are able to automatically interpret the cardiac rhythm, and will only deliver electricity if the rhythm is “shockable.”
As soon as a defibrillator is available, it should be used to check the cardiac rhythm. For AEDs, the rhythm check will be automatic. For full-function hospital defibrillators, there is generally an option for automated rhythm interpretation, or trained rescuers can visually identify the rhythm. The immediate goal is to determine if the rhythm is shockable. Shockable rhythms in cardiac arrest include ventricular fibrillation and ventricular tachycardia.(Ref.7) See sections below for more information on rhythm identification.
As soon as a shockable rhythm is identified, defibrillation should be performed.(Ref.7) Defibrillation is an untimed electrical stimulus delivered to the heart, and in adult patients with cardiac arrest, it is given at the highest possible dose of energy (200J on modern biphasic defibrillators). Defibrillation may be contrasted to cardioversion, which is a timed electrical stimulus that is often given at a lower dose of energy, used to convert abnormal rhythms in patients who have a pulse. Cardioversion is never used in cardiac arrest.
After chest compressions, defibrillation is the most important determinant of outcome in cardiac arrest, and should never be delayed for any reason. As soon as a defibrillator is available, using it is the top priority. Continue compressions as much as possible while attaching the defibrillator, but do not allow any other interventions to interfere. As soon as the defibrillator is attached and turned on, pause compressions to check the rhythm, and deliver a shock if indicated.(Ref.7)
The importance of high-quality CPR and early defibrillation cannot be overemphasized. The time that elapses between cardiac arrest and defibrillation is one of the most important determinants of patient outcome, as every minute without defibrillation is associated with a 7-10% decrease in the likelihood of survival. High-quality CPR slows this decline in survival outcomes.(Ref.8)
Presentation
Cardiac arrest is not a subtle clinical presentation. Patients are universally unresponsive and pulseless. In the peri-arrest period, they may have some agonal breathing, but by the time they are in cardiac arrest, they will be apneic as well. All unresponsive patients in whom a carotid pulse cannot be confirmed within 10 seconds should be assumed to be in cardiac arrest.
Diagnostic Testing
There are no tests needed to confirm the diagnosis of cardiac arrest. However, management of cardiac arrest patients varies by cardiac rhythm. For this reason, accurate interpretation of the rhythm during the arrest is essential. AEDs can determine if a shockable rhythm is present, but clinicians should also be able to recognize and differentiate between rhythms in cardiac arrest.
There are three basic categories of cardiac arrest rhythms:
- Ventricular fibrillation(VF)/pulseless ventricular tachycardia (pVT)
- Pulseless electrical activity (PEA)
- Asystole
Each of these are treated according to different algorithms.
Ventricular Fibrillation and Pulseless Ventricular Tachycardia:
VF and pVT are treated identically in cardiac arrest. They are both ventricular dysrhythmias that respond well to electricity, and are thus termed the “shockable” rhythms. VF can be recognized by its lack of pattern or predictability. There is a complete lack of organization, and no identifiable P-waves, QRS-complexes, or T-waves. It is most commonly seen in ischemic heart disease, but can be seen in patients with cardiomyopathies or congenital electrical conduction disturbances:

VT, on the other hand, can be recognized by a rapid, regular rate and wide QRS complexes. Typical VT is monomorphic, meaning that all the QRS complexes look the same. It is seen in the same patients as VF:
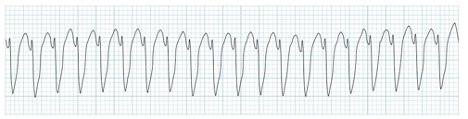
Figure 2: Monomorphic Ventricular Tachycardia. Image courtesy of Life in the FAST Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Original image located at Monomorphic-ventricular-tachycardia-VT.jpg (1010×257) (litfl.com).
VT can also be polymorphic, meaning that the QRS complexes vary in appearance from beat to beat. The “classic” polymorphic form of VT is torsades de pointe, or “twisting of the points.” This name comes from the resemblance of this rhythm to a twisted party streamer, caused by the cyclically increasing and decreasing amplitude of the QRS’s. Torsades is often faster than monomorphic VT (rates >180), and is associated with systemic conditions like electrolyte disturbances or certain toxic ingestions. It can also be seen in patients with congenital electrical conduction disturbances, but is much less common in ischemic heart disease:
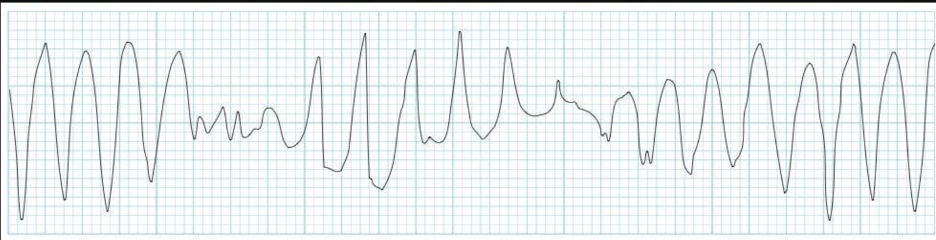
Figure 3. Torsades de Pointes. Image courtesy of Life in the Fast Lane and used under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Original image located at: ECG-strip-Torsades-de-pointes-TDP.jpg (1008×253) (litfl.com).
Pulseless Electrical Activity:
PEA quite literally means the presence of a rhythm in the absence of a pulse. Once VF and pVT have been excluded, ANY rhythm in a patient without a pulse is classified as PEA. The rhythms observed in actual practice are most commonly sinus (in early PEA) or agonal rhythms (in later PEA):
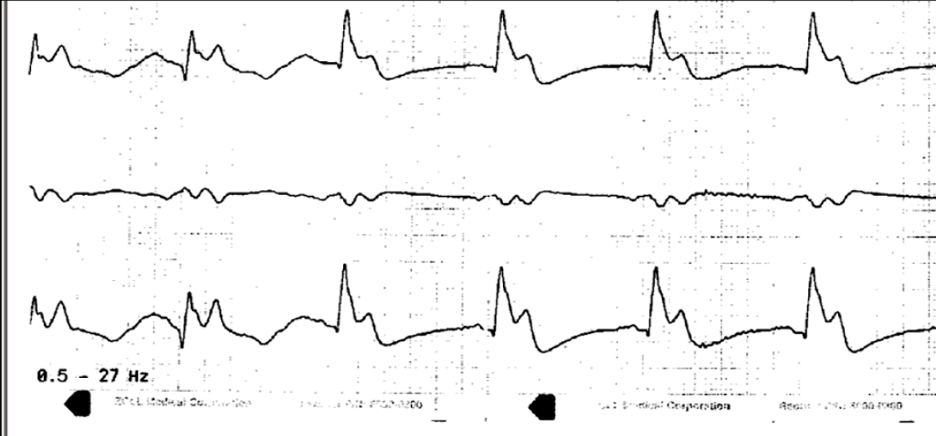
Figure 5. An example of PEA. Image courtesy of Dr. Stephen Smith and used under the Creative Commons Attribution-NonCommercial 4.0 International License. Original located at: Dr. Smith's ECG Blog: 30 Year Old with Cardiac Arrest, PEA, then Cardiac Ultrasound (hqmeded-ecg.blogspot.com).
Asystole:
The final “rhythm” to consider in cardiac arrest is asystole. Asystole is characterized by a flat line with no inflections of any type. It is important to confirm asystole in multiple EKG leads, as a broken or disconnected lead could mimic asystole:
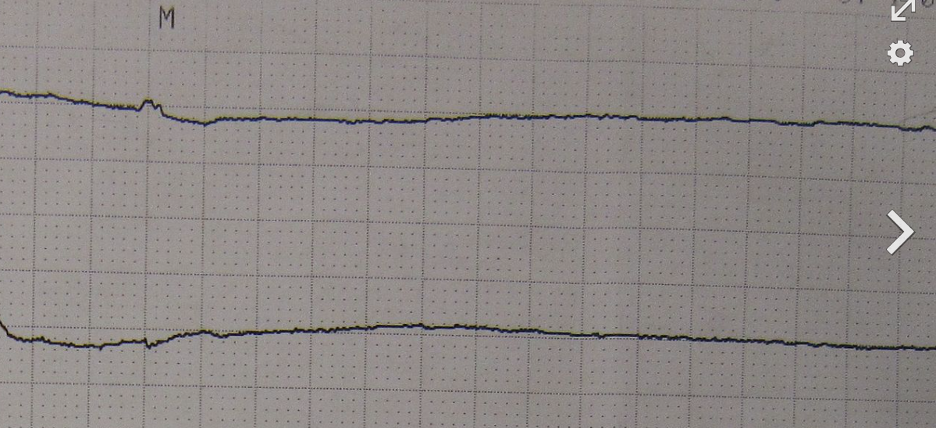
Figure 5. Asystole. Image by James Heilman, MD. Image used under the CC BY-SA 3.0. Original image located at: Asystole11 - Asystole - Wikipedia.
Treatment
Initial treatment:
- Check responsiveness:
- If responsive, patient is not in cardiac arrest - proceed accordingly
- If NOT responsive, check carotid pulse
- Check pulse for maximum of 10 seconds:
- If pulse is clearly present, check respirations and support if needed
- If pulse is NOT clearly present, begin chest compressions immediately
- Once chest compressions have begun:
- Call for a defibrillator
- While waiting for defibrillator to arrive and be set up, begin respiratory support
- Respiratory support:
- Open airway - this can be done using the head-tilt/chin-lift technique and/or jaw thrust.
- Initiate bag-valve-mask ventilation
- Inflate the bag ONLY until you see visible chest rise - you do not need to give high tidal volumes, as this will raise interthoracic pressure, which in turn reduces venous return to the heart and cardiac output
- Coordinate compressions and breaths with a 30:2 ratio, allowing a full second for each inhalation and exhalation
- If you are having trouble getting chest rise, use two-person bag-valve-mask technique, or place an oropharyngeal airway
- Once the defibrillator arrives and is set up, use it!
- Don’t delay defibrillation for ANY reason - do compressions while you’re setting it up, but don’t let any other intervention interfere with defibrillation!
- In shockable rhythm arrests, every minute that goes by without defibrillation decreases the chance of survival
Once the defibrillator is available, you will identify whether the rhythm is shockable. For shockable rhythm arrest:
- The rhythm is either VF or pVT - these are interchangeable in cardiac arrest, and are treated exactly the same. Note that VT can occur either with or without a pulse - this discussion is only pertinent to pulseless VT! Management of VT with a pulse is addressed in a different chapter
- When a shockable rhythm is identified, defibrillation is the first and most important intervention:
- Charge defibrillator to highest setting (200J for biphasic defibrillators, which are used in virtually all US hospitals)
- Continue chest compressions during charging - reduction of the “preshock pause” has been associated with improved outcomes
- Once the defibrillator is fully charged, clear the patient
- Deliver the shock
- Immediately resume CPR
- Continue CPR for 5 cycles of 30:2 compressions:breaths, or for 2 minutes by the clock. Do not check the rhythm again until then!
For non-shockable rhythm arrest:
- The rhythm is either PEA or asystole - their management is similar in cardiac arrest, except that PEA is much more likely to be treatable than asystole. Asystole can be thought of as “end-stage” cardiac arrest, and is not commonly associated with successful resuscitation
- Provide high-quality chest compressions coordinated with ventilation as above
- Defibrillation is NOT used - this may seem obvious, but non-shockable rhythms are not treated with electricity!
- Instead, consider reversible causes of arrest, and treat them if applicable. The differential diagnosis of PEA is known as “the H’s and T’s,” outlined in the charts below.
The H’s | ||
Diagnosis | Evidence | Treatment |
Hypovolemia/ hemorrhage | H/o trauma, fever, vomiting/diarrhea Bleeding, pallor, poor skin turgor, dry mucous membranes Ultrasound - IVC measurement, RUSH exam | IV fluid Blood transfusion |
Hypoxia | H/o preceding dyspnea or pulmonary disease Abnormal breath sounds Cyanosis, low SpO2 (if detectable) | Basic airway maneuvers OR intubation Mechanical ventilation Increase FiO2 and PEEP to optimize oxygenation |
“H+ Ion” (Acidosis - unusual as primary cause of arrest but may contribute) | H/o preceding illness that may affect acid/base balance (e.g., DKA or severe COPD) VBG or ABG, ETCO2 value | Optimize ventilation Bicarbonate Address underlying cause |
Hyperkalemia or Hypokalemia (much less common) | H/o preceding illness with volume loss H/o renal failure, dialysis line or fistula ECG changes | HyperK: Calcium chloride, insulin/glucose, albuterol, bicarbonate HypoK: replete K and Mg |
Hypothermia | H/o environmental exposure Cold skin, low rectal temperature | Passive and active rewarming techniques |
Table 1. The H’s.
The T’s | ||
Diagnosis | Evidence | Treatment |
Thrombosis, Pulmonary | H/o prior PE or PE risk factors Unilateral leg swelling | Thrombolysis Embolectomy (if stabilized) |
Thrombosis, Coronary | H/o preceding chest pain ECG | Thrombolysis Percutaneous coronary intervention (if stabilized) |
Tamponade | H/o preceding thoracic trauma OR condition that causes pericardial effusion (uremia, autoimmunity, cancer, etc.) Jugular venous distension Ultrasound of heart | Pericardiocentesis |
Tension Pneumothorax | H/o preceding trauma OR condition that causes pneumothorax (COPD, cystic fibrosis, pneumocystis, pulmonary fibrosis, etc.) Unilaterally absent breath sounds Tracheal deviation, chest wall crepitus | Needle decompression Tube thoracostomy |
Toxins | H/o substance ingestion or suicide attempt Pupil and skin exam | Drug-specific antidotes General supportive care |
Table 2. The T’s. Charts adapted from Hillman, Cardiac Arrest, CDEM Curriculum, 2015.
Advanced Interventions
After high-quality chest compressions are underway and defibrillation has been performed, it is time to begin advanced interventions including endotracheal intubation, vascular access, and administration of parenteral medications. While these interventions are termed “advanced,” they are actually much less important than the “basic” treatments described above, and only contribute marginally to survival outcomes.(Ref.9)
Airway management:
An advanced airway should be secured only once there is sufficient manpower and expertise to do so without interrupting chest compressions or defibrillation. Endotracheal intubation does not improve survival outcomes, and is not a mandatory intervention for cardiac arrest patients. It is performed as a convenience, permitting reliable respiratory support without the challenges of positioning and mask seal that are inherent to bag-valve-mask ventilation.
Once an advanced airway is placed, it is no longer necessary to coordinate compressions and breaths. Compressions can be continuous, while breaths are given every 6 seconds, or 10 per minute. It is prudent to use 100% oxygen to ventilate (10-15L flow) until such time as a reliable pulse oximetry tracing can be obtained.
Vascular access:
Peripheral intravenous (IV) placement is the first choice for vascular access in cardiac arrest. If a peripheral IV can’t be placed quickly, then intraosseous (IO) access should be obtained. The humerus is preferred for IO access in cardiac arrest but the tibia can be used as well, provided there is no trauma below the diaphragm. Central lines generally are not necessary in cardiac arrest, and their placement can interfere with more important interventions such as chest compressions. However, in the case of arrest due to blood loss or extreme volume depletion, a large-bore femoral line may be considered for rapid administration of large quantities of IV fluid or blood.
Medications:
Epinephrine: This is the only medication that is indicated in all types of cardiac arrest: VF/pVT, PEA, and asystole.(Ref.7) It is a vasopressor, and its function is to vasoconstrict the periphery, allowing preferential perfusion of the heart and the brain. Epinephrine has been associated with improved rates of return of spontaneous circulation (ROSC).(15) However, it has been shown not to improve rates of survival to hospital discharge, and may worsen neurologic outcomes.(Ref.16) In a meta-analysis, epinephrine was shown to have greater benefit in nonshockable arrest rhythms.(Ref.17) This is not surprising, as epinephrine increases cardiac rate, contractility, and automaticity - all deleterious effects in patients with ischemic coronary disease or ventricular dysrhythmias like VF/pVT. Study of the optimal role of epinephrine is ongoing, but current guidelines recommend 1mg of 1:10,000 solution given IV/IO every 3-5 minutes throughout the arrest. The first dose should be given as soon as IV access is available, as early administration has been associated with improved survival outcomes.(Ref.18)
Other Medications:
- Magnesium is the drug of choice for torsades de pointe.
- Calcium, insulin/dextrose, albuterol, and bicarbonate may be used for hyperkalemia.
- Bicarbonate may also be used for severe acidosis and for some toxic ingestions.
- Thrombolysis may be used for massive myocardial infarction or pulmonary embolism.
- IV fluids and/or blood may be given for hypovolemia.
- Atropine was historically used for asystole and slow PEA, but this is no longer recommended due to lack of efficacy.(Ref.7)
Post-Arrest Care:
Care following cardiac arrest is complex, and a complete discussion is beyond the scope of this chapter. However, there are a few important principles to keep in mind:
- Respiratory Support: If an advanced airway wasn’t placed during the resuscitation, it should be considered now. All unresponsive patients should be intubated, while those who are awake and alert generally do not need airway support. Oxygen saturation should be maintained above 93%.
- Vasopressor Support: Hypotension is very common after cardiac arrest. In most cases, this is caused by cardiogenic shock, either from the cardiac event that led to the arrest, or from the ischemic insult of the arrest period. In most cases, vasopressors are the treatment of choice for hemodynamic support. For patients with mean arterial pressures (MAP) under 65, vasopressors should be provided to keep MAP at 65-70, but not higher. Vasopressor doses should be kept as low as possible to prevent adverse events like ventricular dysrhythmias. In some cases hypovolemia may be present, so volume status should be assessed, and judicious IV fluid may be used as appropriate.
- Targeted Temperature Management: Several years ago, therapeutic hypothermia was very popular for post-arrest patients. It is now known that preventing hyperthermia is more important, and patients do equally well whether their temperatures are regulated in a low or near-normal range.(Ref.20) Monitor patient temperatures closely, and avoid hyperthermia.
- Percutaneous Coronary Intervention (PCI): Ischemic coronary disease is a common cause of cardiac arrest, and PCI should be considered for all stabilized post-arrest patients. Obtaining a 12-lead ECG is mandatory in patients who are successfully resuscitated from cardiac arrest, and timely PCI should be performed if an ST-segment elevation myocardial infarction (STEMI) is identified.(Ref.7) Studies have shown that when PCI is performed on all post-arrest patients regardless of ECG, survival outcomes are improved. This is thought to be related to poor sensitivity and specificity of ECG criteria for STEMI in the post-arrest period.(Ref.21) It is therefore reasonable to consider PCI for all patients, though it is only required to perform it in those with confirmed STEMI.
Pearls and Pitfalls
Pearls:
- Always check pulse at the carotid artery - it’s the most central pulse, and the last to be lost when circulation fails. It is thus the most “sensitive” test for pulselessness!
- Remember that cardiac output is the product of heart rate and stroke volume. Anything that impairs either of these will also reduce cardiac output:
- CO = HR x SV
- HR is determined in cardiac arrest by compression rate - PUSH FAST (100-120 beats per minute) to optimize this part of cardiac output (Ref.10)
- SV is determined by compression depth - PUSH HARD (2-2.5 inches) to optimize this part of cardiac output (Ref.11)
- Remember that cardiac filling depends on venous return to the heart, which in turn depends on negative interthoracic pressure. Anything that raises interthoracic pressure (like excessive ventilation or leaning on the chest between compressions) will also impair SV (Ref.12)
- Excessively fast compressions impair SV by reducing filling time - push fast, but not too fast! Ideal rate is 100-120
- Defibrillate as soon as possible for shockable rhythms! Chest compressions are important, but they are just temporizing the situation until the heart restarts - this is what defibrillation will (hopefully) accomplish.
- VF/pVT are usually caused by primary cardiac causes like myocardial infarction, but PEA is more likely to be associated with a noncardiac cause like electrolyte disturbance, volume depletion, or ingestion. In PEA, the key to success is identifying and reversing the underlying cause!
- Focus on the basics! Chest compressions, defibrillation, and reversing underlying causes are the most important interventions. “Advanced” treatments like intubation and administration of medications generally play a small role in cardiac arrest outcomes.
Pitfalls:
- Don’t worry too much about breathing…except when you should!
- Most cardiac arrest patients have normally functioning lungs before the time of arrest. If they are oxygenating normally before the arrest, they will have a reserve of dissolved oxygen in the blood. They won’t begin to desaturate for at least a few minutes
- However, if a patient arrests because of asphyxia, they are starting the arrest with that oxygen reserve depleted. This means that all of your chest compressions will just circulate deoxygenated blood - so you need to support respiration much sooner. Consider this in patients with drowning or any pulmonary cause of arrest.
- Don’t stop compressions except when absolutely necessary (i.e., scheduled rhythm check)! Greater continuity in compressions has been associated with better survival outcomes.(Ref.13,14) Stopping compressions stops blood flow to the heart and the brain, and worsens overall perfusion, as can be seen in this diagram:
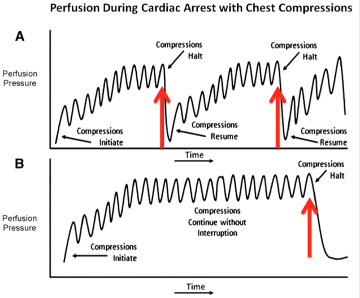
Figure 6. Perfusion during chest compressions. Image courtesy of R.E.B.E.L. EM (Salim R. Rezaie, MD) /. Used under the Attribution-Noncommercial-NoDerivs 3.0 Unported Creative Commons license (CC BY-NC-ND 3.0).
Case Study Resolution
You are now ready to take control of the chaos. You assign one team member to chest compressions, monitoring the quality closely. You ask another to set up the defibrillator, and when it’s ready you discover the patient is in VF. You defibrillate and resume CPR, but wait! Is the patient moving his arm? He opens his eyes and asks what happened. As you reassure him, you notice huge ST-elevations on the monitor, and ask for an ECG. Your attending is already on the phone getting in touch with the cath lab. As you work on stabilizing him for transport, you realize that this man is alive because of you!
References
- CPR & Sudden Cardiac Arrest (SCA) Fact Sheet. (2014, September 3). Retrieved June 3, 2015 from http://www.heart.org/HEARTORG/CPRAndECC/WhatisCPR/CPRFactsandStats/CPR-Statistics_UCM_307542_Article.jsp
- American Heart Association Emergency Cardiovascular Care Committee. (2010). 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 122:S639–946. doi: 10.1161/CIR.0b013e3181fdf7aa
- Heart Disease and Stroke Statistics—2015 Update A Report From the American Heart Association. (2014). Circulation, 131, E29-E322. doi:10 .1161/CIR .0000000000000152
- Heart disease and stroke statistics - 2020 Update: A report from the American Heart Association. Circulation, 2020;141:e-139-596. https://doi.org/10.1161/CIR.0000000000000757
- Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: Incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33(2):237-245.
- Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39(11):2401-2406. (Epidemiologic registry study, 433 patients)
- Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 2020; 142:S366-S468. https://doi.org/10.1161/CIR.0000000000000916
- American Heart Association Emergency Cardiovascular Care Committee. (2015). Highlights of the 2015 American Heart Association Guidelines Update for CPR and ECC (Ebook ed., pp. 1-33). American Heart Association.
- Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009 Nov 25;302(20):2222-9.
- Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, Powell J, Daya M, Bigham BL, Atkins DL, Berg R, Davis D, Stiell I, Sopko G, Nichol G. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012 Jun 19;125(24):3004-12.
- Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D, Aufderheide TP, Idris A, Stouffer JA, Stiell I, Berg R. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009 Sep 29;120(13):1241-7.
- Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnife S, von Briesen C, Sparks CW, Conrad CJ, Provo TA, Lurie KG. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004 Apr 27;109(16):1960-5.
- Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, Bigham B, Morrison LJ, Larsen J, Hess E, Vaillancourt C, Davis DP, Callaway CW. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012 Apr;40(4).
- Vaillancourt C, Everson-Stewart S, Christenson J, Andrusiek D, Powell J, Nichol G, Cheskes S, Aufderheide TP, Berg R, Stiell IG. The impact of increased chest compression fraction on return of spontaneous circulation for out-of-hospital cardiac arrest patients not in ventricular fibrillation. Resuscitation. 2011 Dec;82(12):1501-7.
- Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011 Sep;82(9):2011 Jul 2.
- Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O'Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018 Aug 23;379(8):711-721.
- Holmberg MJ, Issa MS, Moskowitz A, Morley P, Welsford M, Neumar RW, Paiva EF, Coker A, Hansen CK, Andersen LW, Donnino MW, Berg KM; International Liaison Committee on Resuscitation Advanced Life Support Task Force Collaborators. Vasopressors during adult cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2019 Jun;139:106-121.
- Ewy GA, Bobrow BJ, Chikani V, Sanders AB, Otto CW, Spaite DW, Kern KB. The time dependent association of adrenaline administration and survival from out-of-hospital cardiac arrest. Resuscitation. 2015 Nov;96:180-5.
- Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, Leroux B, Vaillancourt C, Wittwer L, Callaway CW, Christenson J, Egan D, Ornato JP, Weisfeldt ML, Stiell IG, Idris AH, Aufderheide TP, Dunford JV, Colella MR, Vilke GM, Brienza AM, Desvigne-Nickens P, Gray PC, Gray R, Seals N, Straight R, Dorian P; Resuscitation Outcomes Consortium Investigators. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2016 May 5;374(18):1711-22.
- Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kulper M, Pellis T, Stammet P, Wanscher M, Wise MP, Aneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Kaber L, Langergen J, Lilja G, Moller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206.
- Dumas F, White L, Stubbs BA, Cariou A, Rea TD. Long-term prognosis following resuscitation from out of hospital cardiac arrest: role of percutaneous coronary intervention and therapeutic hypothermia. J Am Coll Cardiol. 2012 Jul 3;60(1):21-7.
