COPD
Home
/
About SAEM
/
Academies, Interest Groups, & Affiliates
/
CDEM
/
For Students
/
CDEM Curriculum
/
M4 Curriculum
/
COPD
Author: Paul Zgurzynski, MD. Associate Professor University of Massachusetts School of Medicine
Editor: Navdeep Sekhon, MD. Associate Professor at the Baylor College of Medicine.
Last update: 2019
Case Study
Mary is a 65-year-old female with a past medical history of HTN, CHF, and smoking who presents to the ED by ambulance complaining of three days of worsening shortness of breath and wheezing. Her family called 911 at 4 am after she was unable to sleep at all. On arrival, she is just completing an ipratropium bromide and albuterol nebulizer treatment which helped “a little.” On arrival, patient is sitting upright in the stretcher appearing dyspneic and has cyanotic extremities.
Vitals: BP = 140/90, P = 118, RR = 28, T = 99.3F, O2 Sat = 92% on nebulizer treatment.
Airway: is intact, able to speak a few words
Breathing: Appears labored with audible wheezing.
Circulation: Tachycardic with poor capillary refill, intact pulses.
Disability: Pt is oriented but gripping stretcher and will follow only simple commands.
Exposure: Chest is exposed showing retractions and paradoxical breathing.
Objectives
- Discuss the significance of chronic obstructive pulmonary disease (COPD) in the ED
- Describe the typical patient presentation of a COPD exacerbation
- Understand the routine treatment of a patient with a mild/moderate COPD exacerbation
- Discuss use of adjunctive therapy for severe COPD exacerbation, including non-invasive positive pressure ventilation (NPPV)
- Know the indications for intubation of a COPD patient.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common disease that affects up to 15% of adults. On average, exacerbations of COPD result in 600,000 ED visits per year and is the fourth leading cause of death in adults. COPD is a chronic, mid-life disease that is progressive. There is a broad spectrum of disease from patients with mild symptoms and occasional flares to the patient who is oxygen dependent and frequently hospitalized. Far and away, smoking tobacco is the leading cause of COPD. Worldwide, important secondary causes of COPD include air pollution, use of indoor cooking fires, and alpha-1 antitrypsin deficiency.
COPD is defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) as: “A preventable and treatable disease characterized by the persistent airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lungs to noxious particles or gas.”
COPD exacerbations are the worsening of respiratory symptoms from the baseline of a patient’s disease process. A common trigger for exacerbations are viral or bacterial infections, which account for more than 75% of exacerbations. Other triggers are medications, pulmonary embolisms, hypoxia and weather.
The management of COPD exacerbations is bread and butter for Emergency Medicine, and the Emergency Medicine provider must be adept in its diagnosis and management.
Initial Actions and Primary Survey
Initial actions: Immediately place the ill/potentially unstable patient on the monitor, attach continuous pulse oximetry, and insert an intravenous line.
Airway: Like asthma, the first clinical decision is whether the patient requires immediate intubation. If the patient is unable to protect his/her airway due to somnolence, has markedly ineffective breathing or has severe hypoxia, immediate endotracheal intubation with rapid sequence intubation (RSI) should be performed.
Breathing: Evaluate global work of breathing. Evaluate clinically for signs of respiratory distress or fatigue. Observe for retractions, accessory muscle use and paradoxical breathing. Specifically note respiratory rate. Too fast, > 40/min, is very concerning as well as too slow, <15/min. Evaluate the pulse oximetry reading carefully.
Apply controlled oxygen to all hypoxic patients < 92% who present with suspected COPD. In general, use a controlled delivery system such as a Venturi mask or nasal cannula. Avoid routine use of a non-rebreather mask with 15 L/min of oxygen, unless the patient is not responding to lower flow rates. Some patients retain carbon dioxide and high flow oxygen may cause respiratory depression with the rapid rise in serum PO2 depressing the central ventilatory drive. Giving too much oxygen to a patient with COPD is a common mistake that may result in unnecessary and preventable intubations. Please remember that an O2 sat of 100% in a patient with COPD is likely too high and that you should titrate down the oxygen to maintain their ventilatory drive.
Briefly listen to the lung sounds-- if wheezing/diminished breath sounds, begin nebulizer treatment with beta-adrenergic agonist (albuterol) and anti-cholinergic bronchodilator (ipratropium bromide). Like asthma, early initiation of oral or intravenous corticosteroids may be helpful.
Severely ill COPD patients with increased work of breathing who do not require immediate intubation and are not responding to nebulizer treatments may respond to non-invasive ventilatory support (NPPV).
Circulation: In general, patients with COPD exacerbations will be tachycardic and possibly hypertensive due to increased adrenergic drive. Usually, patients will not be hemodynamically unstable unless there is a complicating factor or diagnosis.
Classic Presentation
A focused history should be obtained quickly from the patient or caregiver. The severity of illness may limit the ability to gather a full history. Mildly affected patient may only note mild dyspnea on exertion. More symptomatic patients may complain of mild to severe dyspnea at rest. Some may only be able to speak one sentence due to breathlessness: “I can’t breathe.” The most severely affected will not be able to speak at all.
The classic symptoms of a patient with a COPD exacerbation includes wheezing, productive cough, dyspnea on exertion, hypoxia, and tachycardia. The patient may relate increased use of inhalers, sputum change, or a new requirement of an upright sleeping position (e.g., chair). In contrast to asthma patients, COPD patients are older and often have multiple co-morbidities and history should also focus on excluding other serious diagnoses such as congestive heart failure, acute coronary syndrome, and pulmonary embolism. For example, sudden onset dyspnea after recent surgery should make a provider consider a pulmonary embolism.
Remember COPD is a chronic illness with ups and downs. Astute ED clinicians will ask their patient and themselves: Why today?
Causes of acute decompensation include:
- superimposed infection
- continued smoking
- non-compliance/lack of medications,
- lack of oxygen therapy (for patients on home O2)
Focused questions can help confirm the correct diagnosis and focus your treatment efforts.
- “Are you currently smoking?”
- “Are you taking your medications/inhalers as prescribed?”
- “What has caused you to come to the ED in the past with your COPD?”
A complete head to toe physical exam should be performed. Physical examination should initially focus on the patient’s overall work of breathing. Look for use of accessory muscles. Look for retractions and respiratory rate. Look for pursed lip breathing and cyanosis. Observe if finger clubbing is present. The lung exam is variable and may reveal wheezing, rhonchi, or even rales. Conversely, the lung sounds may be diminished throughout or even seem absent bilaterally in those with severe emphysema or bronchospasm. Table 1. summarizes common presenting signs and symptoms.
Severely ill patients may appear confused with delirium or have a depressed Glasgow Coma Scale (GCS) due to hypoxia or elevated serum carbon dioxide. In addition to typical findings, those patients affected with cor pulmonale (i.e., pulmonary hypertension) will present with symptoms one may associate as only being present in congestive heart failure: jugular venous distention, leg edema, and hepatomegaly.
Diagnostic Testing
The diagnosis of a COPD exacerbation is made through a thorough history and physical exam. The pulmonary exam is critical to making a diagnosis.
Like an asthma patient, a COPD patient may state to the ED physician the current episode is exactly like a prior episode that improved with standard treatment of oxygen, bronchodilators, steroids, and antibiotics.
However, diagnostic testing in a COPD exacerbation is typically broader than the work-up of an asthma patient. This is because patients with COPD tend to be older and have underlying lung pathology. In addition, patients with COPD tend to have multiple comorbidities, which increase the pretest probability for other disease processes. Avoiding premature closure is key in these patients. As noted, many entities such as CHF, acute coronary syndrome, pulmonary embolus, pneumothorax, pericardial effusion, and pneumonia can all masquerade as an acute COPD exacerbation.
Most patients typically require, at the minimum, a chest x-ray and an electrocardiogram. Unlike asthma patients, many COPD patients need screening laboratory studies to exclude other causes of dyspnea. In severely ill COPD patients, obtaining an arterial or venous blood gas can assist with determining severity of exacerbation /response to therapy
Radiographic Studies

Figure 1. Typical chest x-ray for a patient with COPD. Courtesy of Dr. Yuranga Weerakkody and Dr. Mai-Lan Ho from Radiopaedia.org. (https://radiopaedia.org/, https://radiopaedia.org/articles/chronic-obstructive-pulmonary-disease-1, https://radiopaedia.org/licenchttps://radiopaedia.org/licence). Permission via a modified creative commons license.
A typical chest x-ray may show:
- Lung hyperinflation
- Increased AP diameter
- Flattening of the diaphragm
- Bullous changes
It is important to look at the chest x-ray to assess for other disease processes that may masquerade as a COPD exacerbation such as pneumothorax, pulmonary edema or infiltrate.
Point of Care Ultrasound (POCUS)
Even though point of care ultrasound has limited use in diagnosing COPD exacerbations, it can be helpful in evaluating for other disease processes such as cardiac tamponade, pneumothorax and heart failure.
Electrocardiography
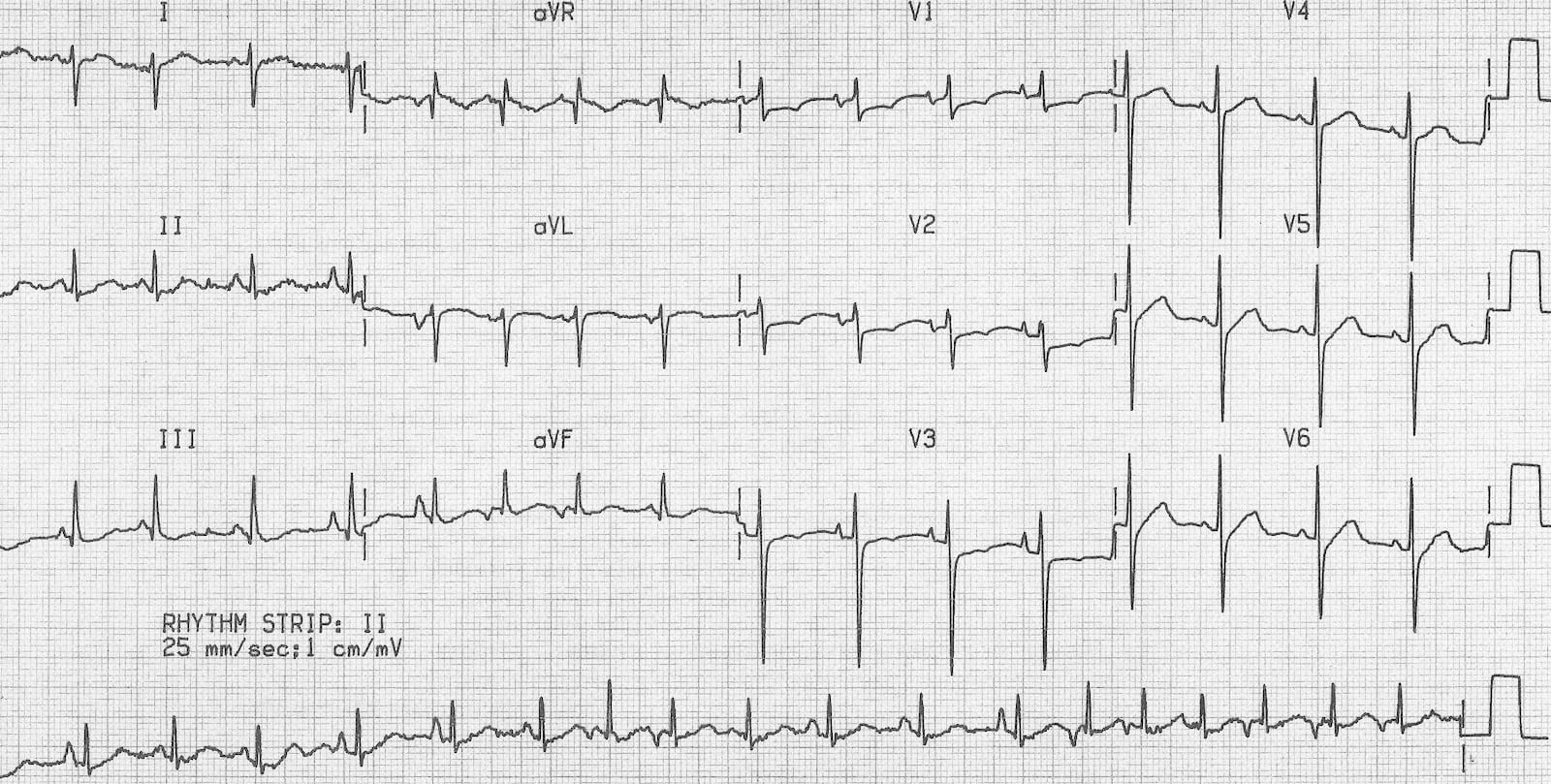
Figure 2. An EKG showing Multifocal Atrial Tachycardia. Courtesy of Life in the Fast Lane EKG Library (https://litfl.com/multifocal-atrial-tachycardia-mat-ecg-library/).
The EKG rarely helps in the diagnosis of a COPD exacerbation, but is frequently necessary to help exclude other disease processes. The EKG may diagnose a significant arrhythmia, STEMI, or show acute ischemic changes suggestive of an acute coronary syndrome. A rare, but specific, finding in COPD patients is multifocal atrial tachycardia (Figure 2)
Common EKG Features of COPD:
- Low voltage, right axis deviation and rightward axis deviation
- P pulmonale- peaked P waves in II, III, aVF
- Right atrial hypertrophy
- Tachycardia
- Multifocal atrial tachycardia (rare, but specific to COPD)
Laboratory testing
While no laboratory test is diagnostic of COPD, several studies may be indicated to exclude other diagnoses based on history and exam. Consider obtaining baseline chemistry and a complete blood count to evaluate for infection and to exclude anemia. Cardiac enzymes and a BNP may be indicated in patients who you suspect are at risk for an acute coronary syndrome or having an element of congestive heart failure. A d-dimer (with subsequent chest CT angiography, if positive) should be considered in patients felt to be at risk for PE or in non-responders to standard treatment.
An arterial or venous blood gas is indicated in moderate to severely ill patients, especially in those not responding to standard treatment with bronchodilators. The blood gas should be evaluated for the degree of hypoxia, acidosis, and CO2 retention. Serial blood gases are frequently necessary to assess trends in the ill patient with a focus on the pH to determine if the patient has decompensated from their baseline. Patients who have severe COPD often have chronically elevated carbon dioxide levels, but those with respiratory failure will develop an acute respiratory acidosis as the pH falls in response to rising carbon dioxide levels. If available, comparison with an old arterial blood gas is extremely helpful. A simple rule of thumb is to remember in an acute respiratory acidosis the pH drops 0.08 for every 10 mmHg rise in carbon dioxide.
Treatment
In general, pharmacologic treatment revolves around the use of beta-2 bronchodilators, inhaled anti-cholinergic agents (ipratropium bromide), corticosteroids (methylprednisolone/prednisone), and antibiotics to treat superimposed infection.
B-2 agonists
Like asthma, the use of beta-2 agonist is first line therapy to get immediate improvement. Inhaled albuterol, the preferred beta-agonist, provides the most rapid response in most patients. A typical dose is 2.5-5mg in 3 ml of saline solution. Even after multiple doses a clinical response may occur. The “continuous” albuterol treatment is 10-20 mg nebulized over a more prolonged period. Limiting factors to ongoing use include tremor, tachycardia, and hypokalemia. In the older adult, other cardiovascular side effects such as cardiac ischemia are possible.
There is no role for long acting beta-agonists such as salmeterol and formoterol in treatment of the acute exacerbation. Long acting beta-2 agonist agents have only been shown to be effective in maintenance therapy.
Anticholinergic agents
Ipratropium is an anti-cholinergic bronchodilation agent, which is also first line therapy in an acute COPD exacerbation. Like asthma, it is typically used as combination therapy (DuoNeb) in nebulized form with albuterol. A typical dose is 0.5 mg in 3 ml of saline. For maintenance it is given every 4-6 hours, but is also used acutely in stacked or repeated doses like albuterol typically for a maximum of 3 doses. Anti-cholinergic side effects such as tachycardia and drying of secretions can occur
Corticosteroids
Systemic corticosteroids are used to reduce secretions and airway inflammation in acute decompensations of COPD. Intravenous (methylprednisolone) and oral steroids (prednisone) are indicated for both moderate and severe COPD exacerbations. Oral and IV steroids are equally efficacious in treating acute COPD exacerbations. Unlike inhaled bronchodilators, the onset of action is delayed and may take up to 12-24 hours to have a clinical effect. Patient with a COPD exacerbation will benefit with a regimen of 5-7 days of systemic steroids.
Corticosteroids have been shown to reduce treatment failure, hospital stay, and the need for additional medical therapy. Some end stage COPD patients are steroid dependent and take daily doses.
Complications of steroid use are more common and clinically significant in older patients.
These complications include:
- elevated blood sugars
- worsening hypertension
- gastritis
- steroid psychosis.
Antibiotics
Empiric antibiotics are used more commonly in COPD than in asthmatic patients. Antibiotics are indicated if signs of infection are present and in patients with moderate to severe exacerbations who are admitted to the hospital. For patients who are discharged, antibiotics should be considered in patients with worsening dyspnea, increased sputum production, and/or increasing purulence of sputum.
Multiple appropriate antibiotic options are available. Common options include macrolides, fluoroquinolones, tetracyclines and cephalosporins. Complications of antibiotics include: allergic reaction, gastritis, and C difficile colitis.
Adjunctive Therapy / Non-Pharmacologic for Decompensated Patients
Continuing respiratory decompensation with worsening carbon dioxide retention and hypoxia despite standard treatment are indications for adjunctive therapy with non-invasive positive pressure ventilation (NPPV) or endotracheal intubation.
The decision to initiate one of these adjunctive therapies can be a purely clinical one based on overall assessment of work of breathing, or via direct measurement of arterial blood gases. There is no absolute guideline for a specific level of built -up carbon dioxide and it is not uncommon for severely affected patients to be awake and relatively stable with a PC02 over 60mmHg. However, worsening acidosis < 7.36 and persistent hypoxia are good markers for the need to consider adjunctive therapy.
Non-invasive positive pressure ventilation (NPPV) is a mode of mechanical ventilation given by facemask that aids oxygen delivery and decreases work of breathing. It is the next logical step in therapy for the patient not responding to standard treatment. However, it should be started early before acute neurologic deterioration or respiratory depression occurs. An experienced respiratory therapist is invaluable in managing these patients and will help guide the clinician in determining the optimal oxygen flow and pressure settings. BiPAP is the preferred mode of NPPV in COPD. A Cochrane review of 14 studies found the following results: NPPV reduced mortality by 50%, decreased the need for intubation, and reduced treatment failure by 52%. Adjustment of the inspired oxygen, peak pressure, and baseline positive expiratory pressure (PEEP) are done based on the clinical response, but a typical starting setting is 12cmH2O over 5 cmH2O. Non-invasive positive pressure ventilation (NPPV) should be offered to patients with exacerbations when, after optimal medical therapy and oxygenation, respiratory acidosis (pH <7.36) and/or excessive breathlessness persist. It is also important to note the contraindications to BiPAP before applying it to a patient (Table 4). If a patient is unable to tolerate BiPAP, high flow nasal cannula may be helpful.
Rapid sequence intubation (RSI) may be necessary for airway control, correction of hypoxia, and correction of carbon dioxide retention. After intubation and sedation, the ventilator is set with a tidal volume of 4-5 ml per kg of ideal body weight (best calculated by length measurement of the patient). The initial oxygen flow is typically 50-100% depending on pulse oximetry and blood gas measurement. The initial mode of ventilation is typically assist control with a fixed number of ventilations being delivered even if the patient is paralyzed or taking insufficient breaths per minute
General ventilator guidelines include: correcting acidosis, correcting hypoxia, avoiding high peak and plateau airway pressures by ongoing use of bronchodilators and aggressive suctioning of secretions. In the COPD patient, peak pressures may also become increased due to a breath stacking phenomenon (Auto-PEEP). The elevated pressure is relieved by disconnecting the endotracheal tube and then restarting mechanical ventilation with a more prolonged expiratory phase or decreasing the minute ventilation.
Disposition
Ultimate disposition is a clinical decision based on assessment of work of breathing, pulse oximetry, and social support. One simple test is a structured walk around the ED with continuous pulse oximetry. Patients who desaturate significantly or become too dyspneic to complete ambulation cannot be discharged home. Those with moderate exacerbations are admitted to the medical wards for oxygen, steroid, and bronchodilator therapy. Those who require non-invasive ventilation or intubation are admitted to the ICU.
Further explanation of how disposition decisions are reached in patients with COPD exacerbations is provided in the clinical vignettes below. The vignettes outline patients with mild, moderate, and severe disease.
Mild Exacerbation (Outpatient):
John is 45-year-old, >30 pack year smoker, with a history of COPD who presents to the ED with cough, yellow sputum, and a low-grade fever. He has no chest pain. For the past 5 days he has used albuterol at home and has now run out. He has never been intubated or admitted. On arrival the room air oxygen saturation is 94% and the respiratory rate is 20/min. There is moderate wheezing on exam. The chest x-ray is negative. In the ED, he received prednisone, albuterol nebulizer x2, and ipratropium nebulizer with good effect. The patient is discharged on a macrolide, prednisone, and albuterol inhaler. Patient is to follow-up with his primary care physician. Smoking cessation counseling discussed (single most cost-effective intervention).
Moderate Exacerbation (Inpatient):
Alice is 65-year-old smoker with a history of hypertension who presents to the ED with SOB, cough, yellow sputum and chest tightness. The patient slept only about 6 hours in a chair last night. At home, the patient used a nebulizer every 4 hour during the night. In the last 5 years, she has been admitted twice with COPD exacerbations. On arrival, the O2 sat is 91% on room air, the patient is tachypneic to 30/min and there is severe wheezing. A chest x-ray, EKG, and troponin are obtained with no acute changes. In the ED, she received albuterol nebs x 4, nebulized ipratropium, oral prednisone, and oral azithromycin with good effect. After 4 hours in the ED the patient felt much better and tried to ambulate with pulse oximetry monitoring. However, within 1 minute, she desaturated to 86% on room air and became very short of breath. The patient is admitted to the medical floor for further management.
Case Study Resolution: Severe exacerbation (ICU)
Mary is a 65-year-old female with a past medical history of HTN, CHF, and smoking who presents to the ED by ambulance complaining of three days of worsening shortness of breath and wheezing. Her family called 911 at 4am after she was unable to sleep at all. On arrival, she is just completing an ipratropium bromide and albuterol nebulizer treatment which helped “a little.” On arrival, patient is sitting upright in the stretcher appearing dyspneic and has cyanotic extremities.
Vitals: BP = 140/90, P = 118, RR = 28, T = 99.3F, O2 Sat = 92% on nebulizer treatment.
Airway: is intact able to speak a few words
Breathing: Appears labored with audible wheezing
Circulation: Tachycardic with poor capillary refill, intact pulses
Disability: Pt is oriented but gripping stretcher and will follow only simple commands.
Exposure: Chest is exposed showing retractions and paradoxical breathing.
Mary has an 18-gauge intravenous line established, labs are drawn, and she is placed on the monitor in an acute care room. After Mary completes her Duoneb, her room air oxygen saturation is 84% and the respiratory rate is 35/min. She is immediately started on another nebulizer treatment. An EKG is performed showing sinus tachycardia at 115 bpm. Two additional nebulizer treatments and intravenous steroids (solumedrol 125mg) are given with minimal improvement. Chest x-ray shows changes consistent with severe COPD and a focal area of atelectasis versus early infiltrate at the right lung base. Blood cultures are drawn, and a point of care lactate returns at 3.0 mmol/L. Due to concern for possible infection Mary receives broad spectrum antibiotics IV ceftriaxone (1 G) and IV azithromycin (500 mg). Screening labs, including a complete blood count (CBC), basic metabolic panel (BMP), and a troponin are all normal After 30 minutes, BIPAP (IPAP/EPAP:12/5) is applied due to persistent breathlessness and a concerning ABG: pH 7.30, pCO2=65 p02=60 and an oxygen saturation = 90 % while completing her last nebulizer treatment. Gradually over 30 minutes Mary improves with a decreased work of breathing. Three hours later while waiting for an ICU bed and getting serial nebulizer treatments, Mary becomes more somnolent with a decreased respiratory rate. An ABG is obtained with a pH= 7.25, pCO2= 60, a pO2 =59, with an oxygen sat of 89%. A decision is made to intubate with rapid sequence intubation (RSI) and performed without complication. Within 30 minutes the patient is transferred to the ICU for continued care.
Pearls and Pitfalls
- Assess what patient factors may have caused the exacerbation
- Always consider alternate diagnoses such as PE, ACS, pneumonia, and CHF in the COPD patient
- Give titrated oxygen early and give enough. Avoid excessive O2 supplementation as this may cause unnecessary intubations.
- Use a combination of bronchodilators, steroids, and consider antibiotics in moderate and severe exacerbations
- Start NIPPV early in patients who have persistent increased work of breathing
References
Cline, David,; et al. Tintinalli’s Emergency Medicine: a Comprehensive Study Guide. 8th ed. New York, N.Y: McGraw-Hill Education LLC, 2016. Web
Ram FSF, Picot J, Lightowler J, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2004, Issue 3. Art. No.: CD004104. DOI: 10.1002/14651858.CD004104.pub3
Vestbo J, Hurd SS, Agusti AG, et al: Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013; 187: pp. 347-365
Walls, Ron M., Hockberger, Robert S., and Gausche-Hill, Marianne. Rosen’s Emergency Medicine : Concepts and Clinical Practice . Ninth edition. Philadelphia, PA: Elsevier, 2018. Print
