Hypothermia
Update Author: Arleigh Trainor MD USD Sanford School of Medicine Edited
Update Editor: William Alley, MD, RDMS, FACEP Wake Forest School of Medicine
Original Author: Kiran Pandit MD MPH Columbia University, New York New York
Original Editor: Lorraine Thibodeau MD, Albany Medical Center, Albany, New York
Updated November 2019
Case Study
Aaron is a 55-year-old. male who arrives via EMS to your emergency department. It is 2 a.m. and the patient was found intoxicated laying on the street outside of a convenience store. His clothing is wet and his pants are hard and frozen. He is wearing a hat, light jacket, pants and leather boots but no gloves. EMS reports P 60, BP 90/50, RR14, O2 92%. They did not get a temperature. He smells strongly of urine and alcohol. Patient is well known to your institution and is undomiciled and has been kicked out of the last two shelters you placed him in for being intoxicated on the premises. He yells out “Hi Doc” and he rolls past you into his room.
Hypothermia Objectives
Upon completion of this self-study module, you should be able to:
- Identify the aspects of the history and physical exam that raise suspicion for hypothermia and cold injury
- Discriminate degrees of hypothermia by temperature or associated symptoms
- Describe the treatment of the patient with hypothermia or cold injury
Introduction
People with environmental exposure to cold temperatures may present with a variety of signs and symptoms of hypothermia and other cold related injury. Hypothermia is defined as a core body temperature < 35°C. Cold injuries include frostbite and trench foot. As the ED sometimes functions as the safety net for the community, people without the resources or ability to protect themselves from exposure to cold temperatures will often present (or be brought) to the ED for treatment. Patients suffering from hypothermia and cold injury range from outdoor adventurists to intoxicated individuals, the undomiciled, the mentally or physically ill, the elderly, children, and the poor.
This module will discuss only hypothermia caused by the unintentional exposure to cold temperatures (primary hypothermia), not those caused by other disease processes (secondary hypothermia) or therapeutic hypothermia.
Initial Actions and Primary Survey
- Minimize jerky movement of the severely hypothermic patient as movement or exercise may precipitate ventricular fibrillation
- Stabilize airway: endotracheal intubation if needed for airway protection in the unresponsive patient
- Stabilize breathing: administer warm humidified O2, endotracheal intubation for respiratory failure
- Stabilize circulation: monitor, ECG, intravenous access, warm IV fluids
- Remove cold wet clothing, dry patient, cover with warm dry coverings or warming blanket (bear hugger). Initiate active rewarming measures.
- Look for signs of accompanying cold injury, trauma, or underlying illness (secondary hypothermia)
Classic Presentation
Hypothermia: Often environmental exposure is obvious, but atypical cases, such as a wet patient from an indoor environment, are more subtle. Patients with altered mentation may not be able to communicate a history of cold exposure. Bystanders may report a change in personality, paradoxical undressing, rocking, dysarthria, ataxia, or frank confusion.
Frostbite: Cold injury produces damage to exposed extremities, often made worse by poor circulation to the extremity because of constrictive clothing or hypothermia which reduces blood flow to the periphery. Patients first experience pain in the affected areas, then numbness, and may have mistaken the disappearance of pain for improvement.
Trench foot: Lower extremities with prolonged exposure to wet and cold conditions develop tissue damage, often presenting as paresthesias, pain, or numbness.
Physical Exam
Hypothermia: Exam findings do not strictly correlate to temperature, but signs often cluster as hypothermia progresses from mild (32-35oC) to moderate (28-32oC) to severe (< 28oC) (See Table 1).
Table 1. Findings Based on Degree of Hypothermia
Frostbite: Tissues appear pale and firm, with poor capillary refill and sensation. Severe frostbite appears purple due to blood sludging.
Trench foot: Skin may appear red and swollen at first, progressing to blisters and bullae and finally hemorrhage in the skin and deeper tissues.
Diagnostic Testing
The best method for measuring and monitoring core body temperature is a low-reading temperature probe in the esophagus or rectum. Rectal temperature probes (not thermometers) should be inserted five inches into the rectum; lodging the probe in feces will give a falsely low reading. Rectal temperature also lags behind true core temperature during rewarming.
Laboratory testing may reveal hemoconcentration, hypo/hyperkalemia, hypo/hyperglycemia, or abnormal coagulation. Tests that warm blood to 37°C may give false positive or false negative results, e.g. arterial blood gas, coagulation studies.
A plain chest film may reveal pulmonary edema.
ECG may show:
- J (Osborne) waves in moderate-severe cases
- Prolonged intervals (PR, QRS, QT)
- Arrhythmias (atrial or ventricular)
Here is an ECG with Osborne waves in the precordial leads: note the positive deflections at the junction between the QRS and the ST segment.
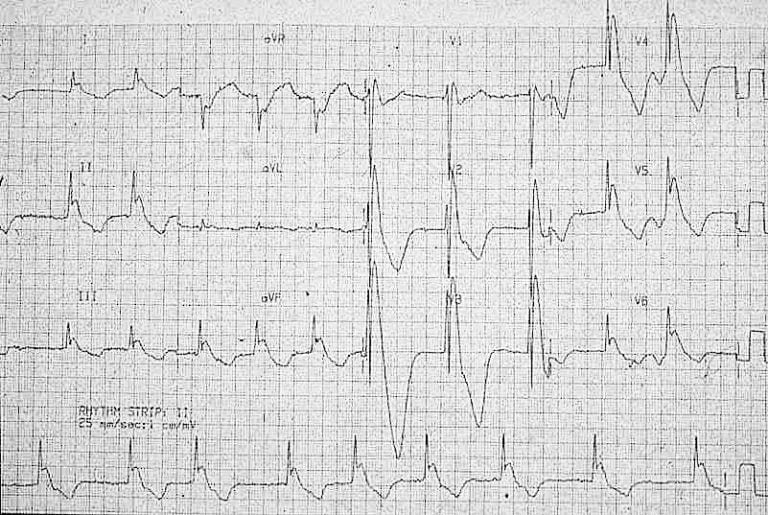
ECG provide from Life in the Fast Lane ECG blog, “Osborne Wave” https://litfl.com/osborn-wave-j-wave-ecg-library/ #FOAMed Medical Education Resources by LITFL is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Frostbite and trench foot are diagnosed by history and physical exam.
Treatment
All wet clothing should be removed and the patient’s skin should be dried. The invasiveness of rewarming methods correlates to the severity of the hypothermia, but rapid rewarming is the goal for all patients.
Table 2. Rewarming Techniques
Most arrhythmias: Provide supportive therapy, not anti-arrhythmics. Cardiac pacing and atropine are often ineffective for bradycardia.
Ventricular fibrillation: Perform CPR and defibrillation per ACLS protocols, except that antiarrhythmics and repeat defibrillation should be deferred until the patient is warmed to above 30oC. Administer bretylium if available. Note that lidocaine is ineffective for hypothermia-induced dysrhythmias.
Resuscitate patients in cardiac arrest while rewarming to a core temperature of 32oC before terminating resuscitation efforts, unless the patient’s chest is frozen or there is ice filling the airway.
Complications of rewarming
The patient’s temperature may decrease during rewarming (called afterdrop) as peripheral vessels dilate and increase return of cool blood from extremities to the core. Rewarming shock (hypotension) may occur as rewarming causes vasodilatation. Rewarming can also drop pH and cause electrolyte imbalances and coagulopathy.
Frostbite: Immediately immerse the affected area in warm water (37-39oC). Remove constricting clothing and jewelry. Consult surgical services for exploration and debridement, though amputation is usually delayed until the gangrenous tissue has clearly demarcated, a process often taking months. Treatment includes ibuprofen as an anti-inflammatory agent, tetanus toxoid, elevation of the affected area, and narcotic analgesia. A potential new therapy is the administration of tissue plasminogen activator to improve perfusion and decrease the incidence of amputation. Observe for the development of compartment syndrome in severe cases. Hypothermia should be treated first before frostbite.
Trench foot: Keep feet warm, clean, and dry. Elevate the extremity.
Disposition
Patients who have suffered from hypothermia and cold injuries must have a warm place to go, and not be discharged back to the cold environment.
Moderate to severe hypothermia often requires care in a monitored or intensive care setting for:
- Close monitoring of core temperature
- Cardiopulmonary support
- Correction of electrolyte and pH imbalances
- Care for comatose or altered patients
- Observation for the development of DIC, rhabdomyolysis, pancreatitis, seizures, and other complications
Pearls and Pitfalls
- Always check a patient’s core temperature in any patient with signs or symptoms consistent with hypothermia.
- Rapid active rewarming minimizes morbidity and mortality.
- Provide aggressive rewarming and resuscitation efforts to patients in cardiac arrest due to hypothermia; they often regain full neurologic recovery.
- Always look for and treat associated injuries and underlying illness.
Case Study Resolution
Patient is moved from the EMS gurney to the bed in the ED. His wet clothing is removed, he is gently dried and 2 large bore IVs are placed with warm fluids started along with a forced warm air blanket being applied. His vitals are T 31C (rectal), P80, BP 95/46, RR12, O2 92%. Airway and breathing are intact. He has normal heart sounds and an EKG shows normal sinus rhythm with no arrhythmias or blocks evident. He is alert and oriented though intoxicated, GCS 15, moves all extremities. His finger tips are pale, cold, and firm, with poor capillary refill and decreased sensation. These are immersed in warm water. His feet are red and swollen but have intact sensation and only minimally delayed capillary refill. He states they are itching and a little sore. He is reassessed and his rectal temperature is now 37C, his feet are improving in color, though there is a single bullae that has developed on the ball of his foot. His fingers are becoming increasingly painful, but still have decreased sensation and capillary refill. Surgery has come down to see him for a consult and he is diagnosed with frost bite of all of his fingers. Patient is undomiciled and there is no shelter that will admit him. He is still intoxicated. As he will need to sober and keep his hands warm and have them monitored, he will be admitted.
References
K Bruen, et al, “Reduction of the Incidence of Amputation in Frostbite Injury with Thrombolytic Therapy,” Archives of Surgery, Vol 142, Jun 2007.
G Giesbrecht, et al, Hypothermia, Frostbite, and other Cold Injuries: Prevention, Survival, Rescue, and Treatment, Second Edition, 2006, The Mountaineers.
“Hypothermia,” 112; IV-136-IV-138, Circulation, Nov 2005.
M Laniewicz, et al, “Rapid Endovascular Warming for Profound Hypothermia,” Annals of Emergency Medicine, Vol 51 No 2, Feb 2008.
“State of Alaska Cold Injuries Guidelines: Alaska Multi-level 2014 Version,” Department of Health and Social Services, Division of Public Health, Section of Community Health and EMS, http://dhss.alaska.gov/dph/Emergency/Documents/ems/documents/Alaska%20DHSS%20EMS%20Cold%20Injuries%20Guidelines%20June%202014.pdf
Brown, DJA, Brugger, H, Boyd, J, Paal, P. Accidental hypothermia. N Engl J Med. 2012;367(20):1930–1938. doi:10.1056/NEJMra1114208
Pasquier, M., Carron, P.N., Rodrigues, A. et al. An evaluation of the Swiss staging model for hypothermia using hospital cases and case reports from the literature. Scand J Trauma Resusc Emerg Med27, 60 (2019) doi:10.1186/s13049-019-0636-0
Yi Hou, Yuanyuan Qiao, Ming Xiong, Dajin Zhang, Wei Rao, Chenghe Shi. (2019) Hypothermia-rewarming: A Double-edged sword?. Medical Hypotheses 133, 109387
Mohamed Nazhat Al Yafi, Michel Alain Danino, Ali Izadpanah, Edouard Coeugniet. (2019) Using Intra-arterial tPA for Severe Frostbite Cases. An Observational Comparative Retrospective Study. Journal of Burn Care & Research 40:6, 907-912.