Venous access
Author Credentials
Author: Khiem Hoang, MD, MPH; Bradley A. Wallace, MD; Todd Taylor, MD; Emory University School of Medicine
Editor: Steven Haywood, MD; Magnolia Regional Health Center (2022 Update), Matthew Tews, DO, MS; Medical College of Wisconsin (Original)
Section Editor: Khiem Hoang, MD, MPH; Emory University School of Medicine
Update: September 2022
*All images courtesy of Emory University School of Medicine unless otherwise cited*
Case Study
A 40-year-old female with a BMI of 50 presents to the ED with altered mental status. She is drowsy with a GCS of 14. POC glucose was 800. Blood gas revealed a pH of 7.15 with a bicarbonate of 12. Multiple nurses tried but could not palpate a vein or obtain
IV access. An external jugular PIV was attempted without success as well. The nurse looks at you and states, “Well doc, I guess it's your turn now!”
Objectives
By the end of this module, the student will be able to:
- Recognize when to utilize ultrasound-guided peripheral IVs (USGPIV) in the ED
- Identify which patients are candidates for USGPIV and which veins to select to optimize the success rate
- List the steps required to complete an USGPIV in both short and long axis
- Understand the difference between short vs long axis when placing an USGPIV
- Recognize the growing role of ultrasound in placing central venous access
- List the steps required to complete an ultrasound-guided central venous catheterization in both short and long axis
Introduction
Both vascular access and bedside ultrasound are vitally important aspects of Emergency Medicine and can often be used in conjunction with one another. Whenever there is difficulty in obtaining peripheral intravenous access by traditional means (i.e., sight or palpation), bedside ultrasound can be a useful adjunct to the procedure and can often succeed when other methods fail. Additionally, using ultrasound at the bedside when obtaining central venous access has become commonplace within Emergency Medicine and throughout the medical field. As vascular access as a whole has been described elsewhere on this site (https://cdemcurriculum.com/vascular-access/), this chapter will focus almost exclusively on using bedside ultrasound as an adjunct when obtaining vascular access.
Ultrasound-Guided Peripheral Intravenous Access
A vast majority of patients in the emergency department will ultimately require peripheral venous access. While venipuncture can be performed on many patients with ease, there are times when obtaining peripheral venous access on patients by traditional
means can prove difficult. In situations such as these, the ultrasound machine is a very useful tool with a high success rate. (Ref.1) Additionally, studies have shown that, when compared to traditional blind venipuncture techniques, ultrasound-guided
peripheral IV access is frequently more successful on the first attempt, requires less time, reduces the number of needle punctures, and improves patient satisfaction. (Ref.2)
Patients on which to consider ultrasound-guided IV access
- Self-proclaimed “hard sticks”
- Patients with end-stage renal disease
- Patients with a history of IV drug abuse
- Obese patients
- Patients with significant edema
- Patients with sickle cell anemia or other blood dyscrasias
- Severely dehydrated patients with poor landmarks
Selecting a Vessel
Location: Sites that are specifically good for ultrasound-guided access include:
- Antecubital fossa
- Basilic vein of the medial upper arm
- External jugular vein

Figure 1. Veins of the arm. By OpenStax College - Anatomy and Physiology, Connexions Web site. Original location: http://cnx.org/content/col11496/1.6/ and https://commons.wikimedia.org/w/index.php?curid=30148290. Used under the Creative Commons Attribution 3.0 Unported License.
Identifying the Vessel
After placing a tourniquet on the patient’s upper arm, use the linear ultrasound probe to evaluate for an appropriate vein making sure to differentiate between vein and artery. The characteristic differentiation between veins and arteries on ultrasound is collapsibility. When applying direct downward pressure with the ultrasound probe, veins should collapse easily while arteries will keep their cross-sectional circular shape; however, note that arteries can often collapse with enough pressure, especially if the patient is hypotensive. Even if an artery partially collapses with pressure, the artery will still pulsate, creating a “winking” appearance.
Clip 1. When gentle downward pressure is applied with the ultrasound probe, veins will easily collapse while arteries will remain patent and often exhibit pulsatility (Torre, J. de la., 2014).
Additionally, arteries will have thicker, hyperechoic walls and pulsatility when compared to veins.

Figure 2. An artery (A) will have thicker, hyperechoic walls (arrows) when compared to veins (V). Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD
If you have identified a vessel that you believe to be a vein but are still uncertain, it can be useful to turn on the ultrasound machine’s color flow. When color flow is turned on, a vein will have a low flow continuous color (or may sometimes be anechoic) while an artery will exhibit a higher velocity pulsatile flow.
Clip 2. The vessel at the center of the clip exhibits pulsatile color flow, indicating that it is an artery. The other vessels in the clip remain anechoic when the color flow is turned on, indicating that they are veins (ABC Vascular Ultrasound, 2019).
Once you have identified a vein, it is important to evaluate its depth and size.
According to a 2010 study by Witting et al., ultrasound-guided IV access is more likely to be successful when the vein is:
- Less than 1.5 cm below the skin
- Greater than 0.4 cm in diameter (Ref. 3)
When attempting to locate an appropriately sized vein, it can be useful to adjust the depth on the ultrasound machine to 2.0 cm or less. The advantages of this are twofold: it decreases attempts at IV placement on veins that are too deep as well as makes superficial veins appear larger on the screen and therefore easier to successfully puncture.
In addition to evaluating the vessel’s depth and size, it is a good idea to scan along the vessel lengthwise to determine its degree of tortuosity. If the vein is exceedingly tortuous it can be difficult to thread the IV catheter. Be sure to scan proximally and distally to your proposed puncture site to evaluate the trajectory of the vein. At times, a vein might be tortuous at a certain region and then become straight or might be too small at a certain region and then get bigger or join another vein. Be sure to follow your vein along its entire course, especially if you are having difficulty locating veins.
Technique
Once you have identified an appropriate vessel as above, two views can be used on the ultrasound machine for peripheral IV placement: short axis (cross-sectional) or long axis (longitudinal). Each method has its advantages and disadvantages, which will be discussed shortly. The supplies needed are the same for either method.
Supplies
- A high-frequency linear ultrasound probe
- Sterile gel/lubricant
- Adhesive dressing (e.g., Tegaderm®)
- IV catheter (ideally longer than 1.16 inches)
- Tourniquet
- Antiseptic solution
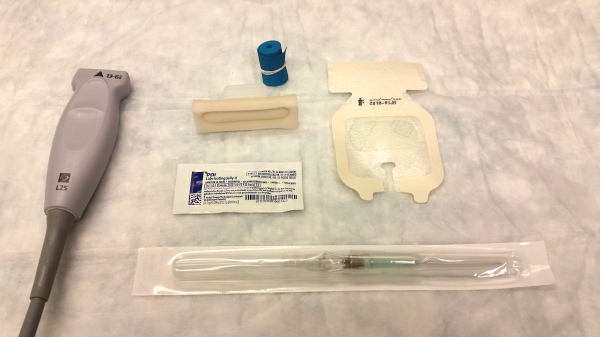
Figure 3. Supplies needed for an ultrasound-guided IV insertion Image Courtesy of Bradley Wallace, MD.
Short Axis (Cross-Sectional) Approach
- Apply tourniquet to the upper arm.
- Cleanse the skin with an antiseptic solution.
- Place adhesive dressing over ultrasound probe to decrease risk of infection. Placing a thin layer of ultrasound gel between the dressing and the probe will prevent damage to the probe caused by the adhesive. A sterile probe cover or sterile glove covering the probe are acceptable alternatives.
- Apply sterile gel/lubricant to ultrasound probe over adhesive dressing
- Place ultrasound probe on skin perpendicular to the previously identified vein making sure to keep the cross-section of the vein at the center of the screen.
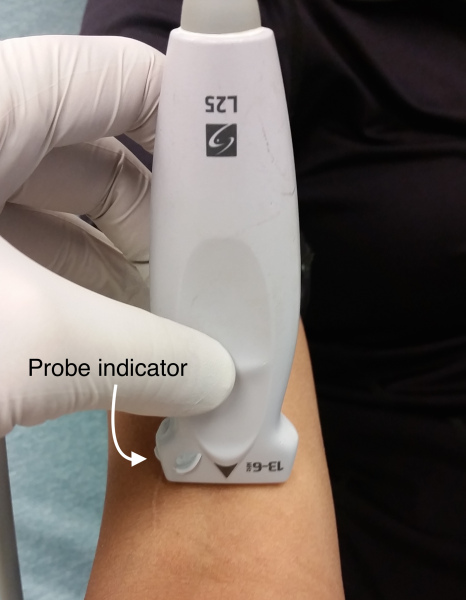
- Ensure that the ultrasound probe indicator is pointing to the patient’s right—i.e., the ultrasound operator’s left—so that the left side of the ultrasound screen corresponds to the ultrasound indicator
- Note that it can be helpful to put a line in the center of the screen that corresponds to the middle of the probe. Some machines have a specific function to do this, while others will require that you activate M-mode. If using this technique, center the line over the chosen vein prior to piercing the skin.
- Pierce the skin at a 45° angle with the catheter at the center of the probe. As soon as you pierce the skin, keep your eyes on the screen!
- Some operators prefer to pierce the skin just proximal to the ultrasound probe and then advance the needle and the probe together.
- Others prefer to pierce the skin more proximal to the probe, using the Pythagorean theorem in an attempt to pierce the vein at the level of the ultrasound probe. When using this technique, it is helpful to understand the 45-45-90 triangle.
 Figure 4. Ratio of side lengths of a 45-45-90 Triangle. Diagram created by Khiem Hoang, MD, MPH.
Figure 4. Ratio of side lengths of a 45-45-90 Triangle. Diagram created by Khiem Hoang, MD, MPH.- If, for example, the vein is 2cm deep, piercing the skin 2cm proximal to the probe at a 45° angle would mean that you should hit the vein after advancing the catheter approximately 2.8cm based on the 45-45-90 triangle above.
- Identify the hyperechoic needle tip on the screen.
- When advancing the needle at a 45 degree angle, the ultrasound waves will be reflected away from the probe making it difficult to visualize the needle. This issue can be resolved by sliding the probe further up the extremity and angling back towards the needle to create a 90 degree angle.
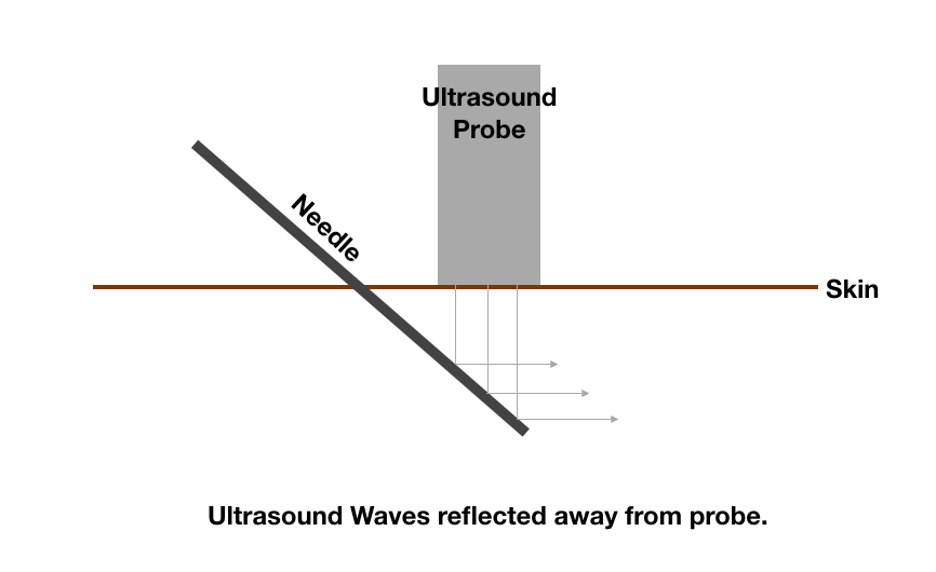

Figure 5. Probe moved and angle adjusted to improve visualization of needle. Diagram created by Steven T. Haywood, MD.
It may be useful to push the catheter up and down or fan the probe back and forth to help identify the needle tip on the screen.
Sometimes you will have to pull back. Make sure you are looking at the screen and follow the tract created to identify the tip and readvance.
Clip 3. The hyperechoic needle tip is visualized proximal/superficial to the blood vessel. Note that when the needle is gently moved back and forth it can be more easily identified (Greg Zahn, 2021).
8. Pierce the vein looking for the “target sign” or “bull’s eye sign” (the hyperechoic needle tip in the center of the anechoic vessel)— you should see a corresponding flash of blood in the catheter once the needle tip has pierced the vessel.
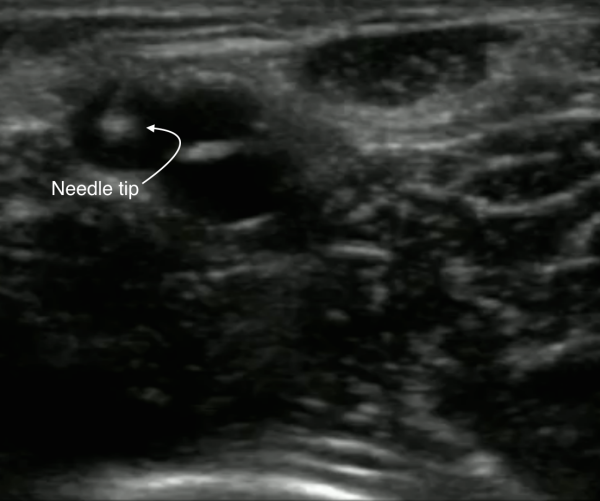
Image 4. Hyperechoic needle tip localized in a blood vessel in short axis. This is called the “target sign” or “bull’s eye sign.” Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD.
9. Once the target sign is visualized, advance the probe proximally until the needle disappears. Drop the tail of the needle and advance until it reappears while keeping the needle tip in the center. Thread the catheter in the usual manner and secure the catheter to the skin with an adhesive dressing.
Since the needle is longer than the catheter, you can get blood return without the catheter itself being in the vein. This is why you should advance the needle by walking more proximally up the vein after obtaining flash before threading the catheter. Dropping the tail of the needle making it parallel to the skin will assure that you do not push through the back wall of the vein as you advance.
10. The IV should now flush easily and painlessly if placed correctly.
To check for extravasation, you can put your hand a bit proximal to the IV while flushing to feel for accumulation of fluid.
Long Axis (Longitudinal) Approach
- Use the same technique as described in steps 1-4 of the short-axis approach above. All of the additional information in the bullet points under each step of the short-axis approach can still apply to the long-axis approach.
- Place the ultrasound probe on the skin parallel to the axis of the previously identified vein with the probe indicator facing toward the patient’s head.

Image 5. Orientation of ultrasound probe for long-axis approach. Note that the probe indicator is pointing towards the patient’s head. Image Courtesy of Bradley Wallace, MD.
3. Pierce the skin at a 45° angle just distal to the ultrasound probe with the needle at the center of the probe.
4. Identify the hyperechoic needle tip on the right side of the screen.
5. Advance the needle tip until you visualize it piercing the wall of the vessel on the screen— you will see a corresponding flash of blood in the catheter once the needle has pierced the vessel.
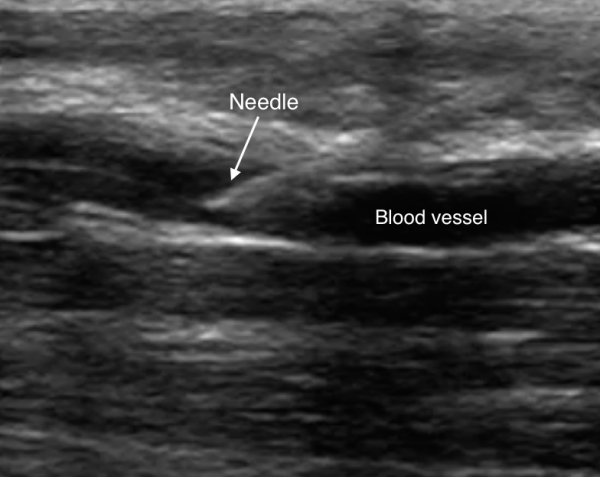
Image 6. Hyperechoic needle tip localized in a blood vessel in long axis. Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD.
6. Drop the tail of the needle to make it parallel to the skin and thread the catheter in the usual fashion and secure the catheter to the skin with adhesive.
7. The IV should now flush easily and painlessly if placed correctly.
Comparison of Methods
Both the short-axis and long-axis approaches have advantages and disadvantages. The main advantage of the short axis method is better lateral resolution (i.e., after piercing the skin, one can tell if the needle tip is lateral to the vein). The main drawback to the short axis technique is the requirement of moving the ultrasound probe dynamically to keep the needle tip on the screen.
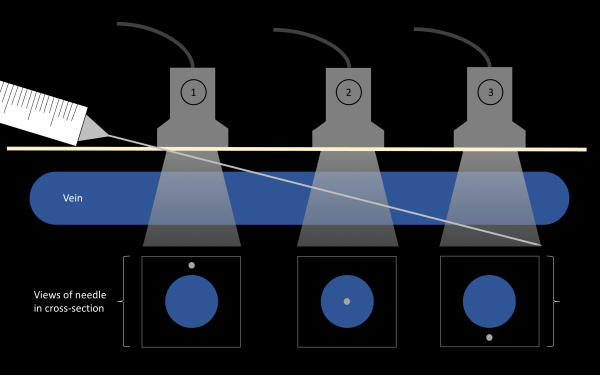
Image 7. In a short axis view, the location of the ultrasound probe can result in the needle appearing to be in multiple different positions. Though the needle in the image above has gone entirely through the vessel, the needle appears to be proximal to the vessel using position 1, within the vessel using position 2, or through the back wall of the vessel using position 3.
Compared to the short axis method, the long axis technique allows the operator to visualize the entirety of the needle and see in real time as it enters the vein in profile, as illustrated in Image 6 above.
While the short axis method has good lateral resolution, the long axis method can be more technically challenging due to its poor lateral resolution (i.e., the needle can appear to be in the same plane as the vessel despite being just lateral to the vessel). Furthermore, with the long axis approach it can be easy to lose sight of the vein and accidentally re-focus the probe onto an adjacent artery with very small moves of the ultrasound probe.
If one is learning the technique for ultrasound-guided IV access for the first time, the short axis approach has been shown to be easier to learn than the long-axis approach for novice operators. (Ref. 4) Furthermore, a 2011 study demonstrated that the short axis method both resulted in a higher success rate and took less time than the long axis approach. (Ref. 5)
The Videos in Clinical Medicine series by The New England Journal of Medicine provides a review of ultrasound-guided IV placement: http://www.nejm.org/doi/full/10.1056/NEJMvcm1005951.
Ultrasound-Guided Central Venous Catheter Placement
While many patients in the emergency department can be successfully resuscitated with only peripheral access, some patients will require central venous access. Though central venous catheters have been associated with certain complications (e.g., pneumothorax, arterial puncture, bleeding, and infection), there have been multiple prospective, randomized controlled trials and several meta-analyses that have shown that the use of real-time ultrasound guidance during catheter placement has reduced the number of complications as well as reducing the number of cannulation attempts when compared to using landmarks alone. (Ref. 6-9)
Note: Central venous access is discussed in depth elsewhere on this site; as such, this chapter will focus on using ultrasound to locate and cannulate central veins. For further information on central venous catheter placement, including indications, contraindications, and the individual steps required for the entirety of the procedure, please refer to the Vascular Access chapter (https://cdemcurriculum.com/vascular-access/).
Location Selection
The three traditional locations for central venous line placement are the internal jugular vein, the femoral vein, and the subclavian vein. The technique for ultrasound-guided central line placement into the internal jugular vein and femoral vein is nearly identical; as such, the discussion here will focus mainly on placement into the internal jugular vein as it tends to be the favored location for central line placement. While the use of ultrasound for subclavian central line placement is becoming more popular, this is a more advanced technique and will not be discussed in this chapter.
Anatomy
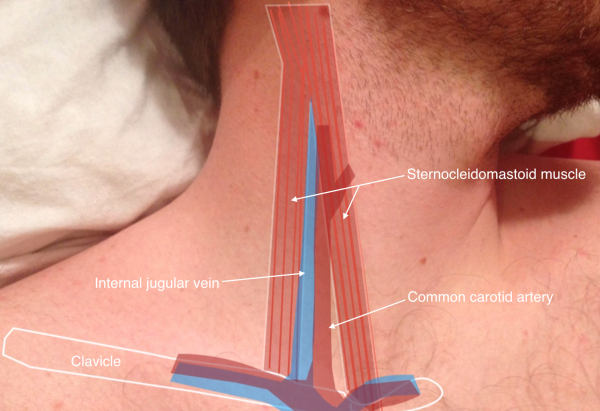
Image 8. Anatomy of major neck vasculature. Both the internal jugular vein and common carotid artery are located in an anatomic triangle formed by the two heads of the sternocleidomastoid muscle and the clavicle. (Image courtesy of Sierra Beck, MD).
Technique
As discussed in the ultrasound-guided peripheral IV access section above, the ultrasound machine can be used to visualize blood vessels in both the short axis and long axis. The materials needed are the same for both, though the technique varies slightly. The short-axis approach will be discussed first.
Supplies
- Central line kit (including drape)
- Sterile gown/gloves/cap
- Probe cover kit (with sterile gel)
- Ultrasound machine with linear probe
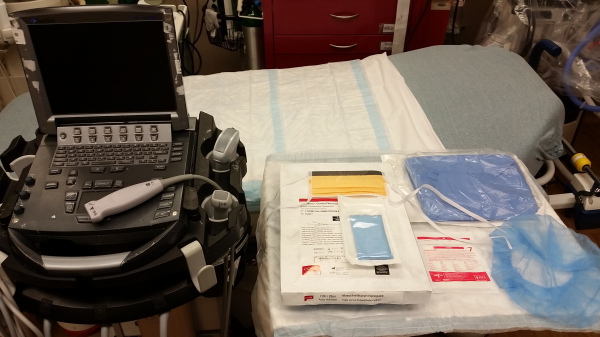
Image 9. Supplies needed for ultrasound-guided central line insertion. Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD.
Short Axis Approach—Internal Jugular Vein
- Standing at the head of the bed, place the ultrasound machine on the patient’s right or left depending on which internal jugular vein you plan to cannulate. Some operators prefer the machine on the ipsilateral side to the internal jugular vein that is being accessed while others prefer the ultrasound machine on the contralateral side— this is largely a matter of personal preference
- Place the patient in Trendelenberg position
- Have patient turn head contralaterally to the desired puncture site
- Apply gel to the linear ultrasound probe
- Place the probe on the patient’s neck just above the clavicle, making sure to have the indicator pointing to the operator’s left side (also patient left) so that the left side of the probe corresponds to the left side of the ultrasound machine
- Walk probe proximally and distally in an attempt to find a site where the internal jugular vein is largest and relatively remote from the carotid artery. Keep in mind that movements of the patient’s head may alter vascular anatomy greatly
- Remember that arteries are typically thick-walled, pulsatile, and non-collapsible when applying pressure with the ultrasound probe while veins are thin-walled, non-pulsatile, and collapse easily when applying pressure with the probe (see Clip 1 and Clip 2 above for how to better differentiate arteries and veins).
- After locating an appropriate puncture site, remove the gel from the patient’s neck and apply the appropriate sterilizing solution (e.g., Chlorhexidine, betadine, etc.)
- Open central line kit, don sterile gown, hat, mask, and gloves, and open ultrasound probe cover
- While you hold the ultrasound probe cover, have an assistant apply ultrasound gel to the ultrasound probe. Proceed to grab the probe with the cover, making sure to keep the probe cover sterile by having the assistant pull the cover through
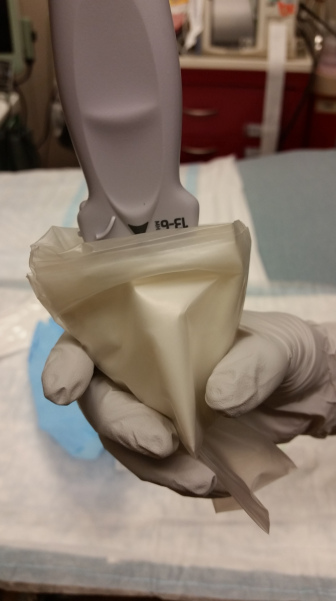
Image 10. Sterile gloved hand holding sterile probe cover open while an assistant places the ultrasound probe into the probe cover. Image Courtesy of Bradley Wallace, MD.
11. Place sterile ultrasound gel on the outside of the probe cover
12. Anesthetize skin overlying the puncture site
13. Place ultrasound on patient’s neck perpendicular to the orientation of vasculature
14. Pierce skin at a 45° angle at the center of the ultrasound probe (keeping the vessel in the middle of the screen) making sure to continuously aspirate immediately after piercing the skin

Image 11. The ultrasound operator is in the foreground with sterile gloves piercing the skin at a 45° angle to the skin at the center of the ultrasound probe. Note that the operator is holding the syringe in a position where they can continuously aspirate once the needle tip has pierced the patient’s skin. In the background of the image, note that the ultrasound image is centered on the hypoechoic internal jugular vein in short axis as the operator is advancing the needle towards the vessel and that the M-mode is on. Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD.
14. Identify the hyperechoic needle tip in relation to the internal jugular vein. It may be useful to fan the probe back and forth or gently bounce the needle up and down in the soft tissue when attempting to locate the needle tip. Be sure to keep the needle tip on the screen by advancing the ultrasound probe along the skin as you advance the needle—this will ensure that you do not inadvertently cannulate the wrong vessel (viz., the artery)
15. Once you note the bull’s eye or target sign (see Image 4 above) you should have aspiration of blood into the syringe
16. When aspiration of blood is confirmed, place the ultrasound probe on the sterile drape, remove the syringe from the needle, and advance the guidewire
17. Remove the needle from the skin
18. Grab the ultrasound probe and place it on the patient’s neck to obtain a longitudinal view of the internal jugular vein. If the wire is appropriately positioned, you will be able to visualize a hyperechoic structure (the wire) in long axis on the ultrasound machine
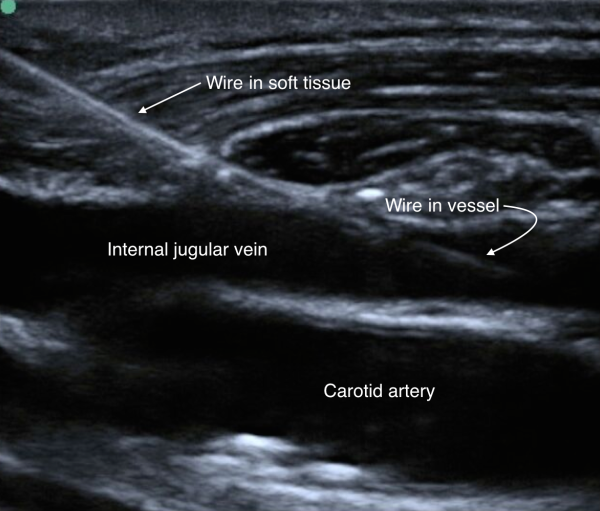
Image 12. Hyperechoic guidewire localized in the internal jugular vein. Image Courtesy of Sierra Beck, MD and Bradley Wallace, MD.
19. Complete placement of the central venous catheter using the Seldinger technique and secure the catheter to the skin
20. Obtain chest X-ray to confirm appropriate positioning of central venous catheter
Long Axis Approach—Internal Jugular Vein
- Carry out the same steps as above (steps 1-13)
- Place ultrasound probe on skin parallel to venous structures when surveying vascular anatomy. Ensure that the probe indicator is oriented towards the patient’s head, corresponding to the left side of the ultrasound screen
- When piercing the skin at a 45° angle, be sure that the entire vessel is visualized on the screen
- With the probe indicator oriented towards the patient’s head, you should see the needle tip enter the left side of the screen after piercing the skin
- Once you visualize the needle tip entering the vessel (see Image 6 above), you should note aspiration of blood into the syringe
- Place probe onto sterile drape, remove the syringe, and thread guidewire
- Place ultrasound probe back onto skin in long axis, attempting to visualize the guidewire within the vessel in long axis— it is critical to verify the location of the guidewire before dilation (see Image 11 above)
- Complete placement of the central venous catheter using the Seldinger technique and secure the catheter to the skin
- Obtain chest X-ray to confirm appropriate positioning of the central venous catheter and ensure that there is no iatrogenic pneumothorax
Note: The femoral vein can be accessed using the same steps as above. When surveying femoral anatomy, remember that the femoral vein is located medially to the femoral artery.
Conclusion
While both peripheral venous access and central venous access were traditionally performed using palpation or anatomic landmarks, the use of ultrasound for both procedures has become more prevalent in Emergency Medicine. Using ultrasound guidance while performing peripheral IV placement has been demonstrated to be a robust alternative to traditional approaches for patients for whom venipuncture has proven difficult while also helping to improve patient satisfaction. Similarly, ultrasound-guided central line placement has been shown to decrease both the number of attempts at cannulation and complications of the procedure. As such, the ultrasound machine should be a consideration whenever contemplating venous access strategies in the emergency department.
Pearls and Pitfalls
- Remember the role of USGPIVs in a patient who needs peripheral access but does not have superficial or palpable veins.
- As with every procedure, preparation is key. Take the time to appropriately position the ultrasound machine in the room and to survey the patient's anatomy to select the best vein to optimize your chances of success.
- As soon as you pierce the skin, keep your eyes on the screen.
- Always visualize the tip of your needle before advancing it. This is why you have the ultrasound!
- Use the middle indicator or M-mode to your advantage. This ensures that you are in line with your target.
- Try to develop proficiency in one method (short vs long axis) before switching to the other.
- Mastering USPGIVs takes practice and patience but troubleshooting them takes understanding the ultrasound and the technique behind the procedure.
- If you can palpate a vein while trying to find one with the ultrasound, try placing a regular IV! Don’t forget to use regular-sized catheters.
Case Study Resolution
With the ultrasound, the physician was able to place two large bore IVs for fluid resuscitation and insulin. The patient’s acid-base status slowly started trending back to normal and her mental status improved. She was admitted to the ICU.
References
- Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999 Dec. 34(6):711-4.
- Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005 Nov. 46(5):456-61.
- Witting MD, Schenkel SM, Lawner BJ, Euerle BD. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J Emerg Med. 2010 Jul. 39(1):70-5.
- Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med. 2003 Dec. 10(12):1307-11.
- Mahler SA, Wang H, Lester C, Skinner J, Arnold TC, Conrad SA. Short- vs long-axis approach to ultrasound-guided peripheral intravenous access: a prospective randomized study. Am J Emerg Med. 2011 Nov. 29(9):1194-7.
- Leung J, Duffy M, Finckh A. Real-time ultrasonographically guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications:a randomized, prospective study. Ann Emerg Med. 2006;48:540-547.
- Karakitsos D, Labropoulos N, De Groot E, et al. Real-time ultrasound guided catheterization of the internal jugular vein: A prospective comparison to the landmark technique in critical care patients. Crit Care. 2006;10:R162.
- Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: A meta-analysis of the literature. Crit Care Med. 1996;24:2053-2058.
- Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, Thomas S. Ultrasonic locating devices for central venous cannulation: Meta-analysis. BMJ. 2003;327:361.
